By Chris Faubel, M.D. —
An acromioclavicular joint injection with fluoroscopy is usually thought to be NOT needed because the joint is typically superficial and is therefore performed “blinded”. But, a study in 2009 showed that of the 76 cadavers injected without fluoroscopy, the skilled, experienced physician did NOT get into the AC joint 42% of the time (1); in comparison, the physician got into the joint 100% of the time when using x-ray guidance.
An alternative to fluoroscopy would be ultrasound guidance, which would eliminate the need for x-ray exposure.
If you perform a “blinded” injection of the AC joint in the clinic and the patient doesn’t get enough pain relief, but you are sure their pain is from the AC joint, consider ultrasound or fluoroscopic guidance, especially if the patient is obese.
Indications
- Acromioclavicular Joint Primary Osteoarthritis and Pain
- ICD-9 code: 715.91 “Osteoarthrosis unspecified whether generalized or localized involving shoulder region”
- ICD-10 code: M19.01 (M19.011, M19.012) “Primary osteoarthritis, shoulder” (right & left, respectively)
- Acromioclavicular Joint (AC) Post-Traumatic Osteoarthritis and Pain
- ICD-9 code: 715.91 “Osteoarthrosis unspecified whether generalized or localized involving shoulder region”
- ICD-10 code: M19.11 (M19.111, M19.112) “Post-traumatic osteoarthritis, shoulder” (right & left, respectively)
- Acromioclavicular (AC) Joint Sprain
- ICD-9 code: 840.0 “Acromioclavicular (joint) (ligament) sprain”
- ICD-10 code: S43.50 (S43.51, S43.52) “Sprain of acromioclavicular joint” (right & left, respectively)
CPT codes:
- 20605 “Arthrocentesis, aspiration and/or injection; intermediate joint or bursa”
- 77002 – Fluoroscopic guidance of a needle (non-spinal)
- Remember to bill for the J-codes for the contrast and steroid as well.
Patient Position
- Supine with arm down by their side
 Materials Needed
Materials Needed
- Gloves – sterile
- ChloraPrep (3-ml)
- Band-aid – small, round
- Needles
- 25-gauge 2″ needle, or a 25-gauge 3.5″ Quincke needle
- 25-gauge 2″ needle, or a 25-gauge 3.5″ Quincke needle
- Syringes
- 3-ml plastic syringe (for the Omnipaque contrast) – use with 6-inch micro-bore plastic tubing
- 3-ml plastic syringe (for the steroid/local mixture)
- Injectate mixture
- 0.5-ml of 40mg/ml Depo-Medrol or Kenalog, or 0.75-ml of Celestone (6mg/ml)
- 0.5-ml of 1% lidocaine or 0.5% bupivacaine
- For skin numbing: Will not need it if using the 25-gauge needle, but can use a tuberculin syringe with 2% lidocaine or ethyl chloride spray.
Tips
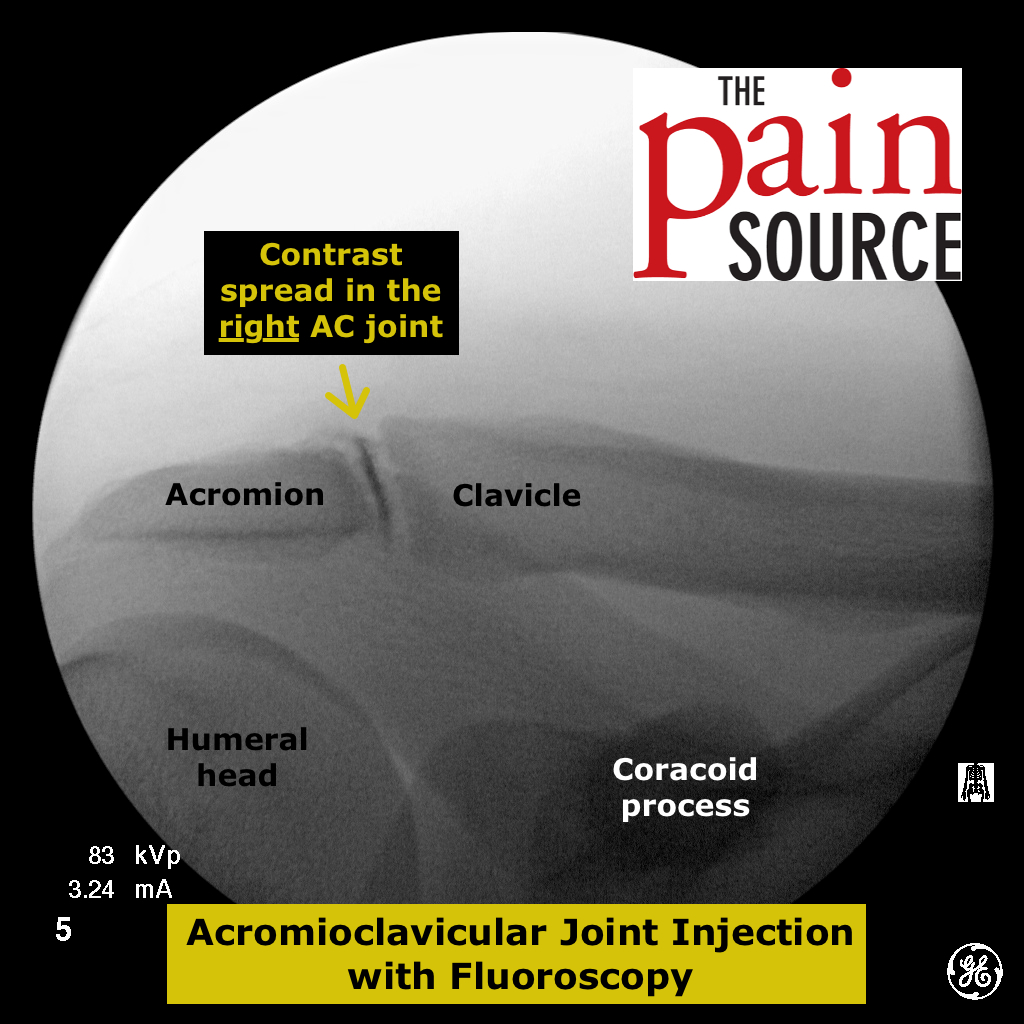
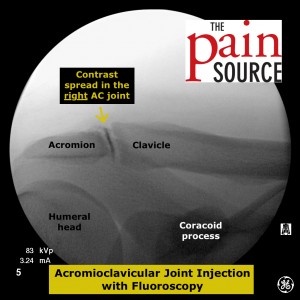
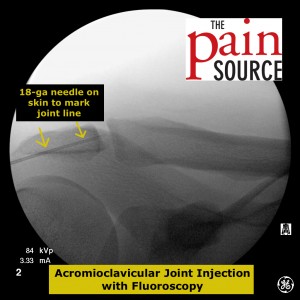
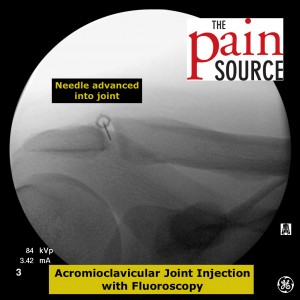
- X-ray tips: Take the time to line up the fluoroscopic image to get a clear shot down the joint line. An ipsilateral oblique is usually needed.
- If the contrast blobs up at the needle tip, adjust the needle.
- Performing this injection in an obese patient with a lot of soft tissue over the AC joint can be dangerous for a potential pneumothorax if no ultrasound or fluoroscopic guidance is used.
References
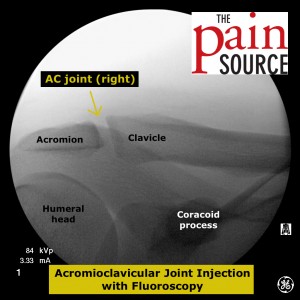 Starting image after doing an ipsilateral oblique tilt of the C-arm in order to get a clear view of the joint line.
Starting image after doing an ipsilateral oblique tilt of the C-arm in order to get a clear view of the joint line.















Whats the position of the patient and the arm?