By Chris Faubel, MD —

Indications
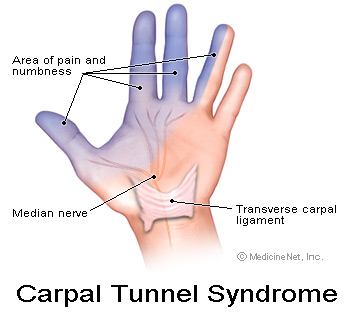
- de Quervain’s tenosynovitis (also called, gamer’s thumb, radial styloid tenosynovitis, De Quervain’s stenosing tenosynovitis)
- ICD-9 code: 727.04 “radial styloid tenosynovitis”
- ICD-10 code: M65.4 “radial styloid tenosynovitis [de Quervain]”
CPT code: 20550 “injection(s); single tendon sheath, or ligament, aponeurosis”
Materials Needed
- Pen – clicking type
- Gloves – non-sterile
- Alcohol swabs or betadine
- Band-aid
- Tuberculin needle/syringe OR 1-ml syringe with 25-gauge 5/8″ needle (depending on body habitus)
- Injectate
- 0.5-ml of 6mg/ml of Celestone OR 0.5-ml of 40mg/ml Depo-Medrol or Kenalog
- 0.5-ml of 1% lidocaine
Technique / Procedure Steps
- Always start with informed consent from the patient, and then a time-out to verify correct patient and injection site.
- Mark the injection site with the pen tip in order to leave an impression in the skin — Point of maximal tenderness (on distal, lateral/radial side of radius).
- Clean the skin thoroughly with as many alcohol swabs as needed (usually only one is needed).
- Patient position: Perform lying supine or seated with the radial side of the wrist up.
- With the tuberculin needle/syringe, enter the skin about 20-30-degrees to the skin.
- Advance until you feel you are under the tendon sheath of the abductor pollicis longus (APL) and extensor pollicis brevis (EPB), but NOT in the actual tendons.
- Aspirate to make sure you’re not in any vessel.
- After negative aspiration, inject the full contents of the syringe, unless lots of resistance is met (means intratendinous needle tip position). Withdraw very slightly, or reposition completely, and try again.
- Withdraw the needle after syringe if fully empty, and apply band-aid.
Tips
- Finding the injection site
- Can gently perform Finkelstein’s test to find the point of maximal tenderness (POMT). For more info on Finkelstein’s test and a great video showing you how to perform it, go HERE
- Numbing the skin
- Find out all about “Taking the Sting Out” (of injections) by going here.
- Since I use a tiny tuberculin needle, most patients have no problem with the injection and don’t need any extra lidocaine skin wheal or freezing spray.
- I tell them numbing the skin with lidocaine will probably hurt more than the actual injection.
- Corticosteroid choice
- Can use Celestone, compounded betamethasone sodium phosphate, or Decadron to minimize the risk for skin atrophy and depigmentation, though many studies showing effectiveness have been done with Kenalog.
- After the injection
- Have the patient ulnarly and radially deviate the wrist a few times while you throw away supplies.
- Then, re-palpate the POMT and have them repeat the Finkelstein maneuver (or regular provocative movement) so they can see the immediate results of the lidocaine.
- Explain to the patient that the lidocaine will wear off in an hour or so, and that they will be back to their normal pain until the steroids start kicking in (anywhere from 1-7 days).
- May also ask the patient to not do much activity with that wrist for 12-24 hours






Use the smallest needle possible that can reach the target point, aspirate, and deliver the steroid…(=
Have a patient who had an odd reaction to dequervain’s injection. Procedure they described is quite different from this post. They reported feeling what they described as great resistance during initial injection and severe pain. A second injection immediately after was given in the thumb. They felt immediate numbness in the thumb, but severe pain remained in the wrist, so much so they were not able to drive home.I am seeing them 4 months post injection with severe atrophy, linear atrophy, parasthesia, hypopigmentation, extreme skin thinning and peeling. Emg results indicate nerve damage.I have not seen such complications before..they have seen another MD for follow up and was told this severe a reaction is “impossible!” They also presented with a new thumb locking which lasted for 2 months and resolved on own-had the appearance of the thumb spontaneously dislocating with severe pain. They never got relief from the injections, but much worse. Any ideas? Thank you..Kerri,OTR
Sounds like they had a DeQuervain’s injection (if it’s intratendinous instead of just under the tendon sheath there can be a lot of resistance…especially if using a tuberculin syringe/needle), and then had either a trigger thumb injection or an intraarticular injection of the 1st carpometacarpal joint. Either way, they shouldn’t have had “nerve damage” from either injection. The “nerve damage” was probably already there. Without a pre- and post-injection EMG/NCS, it’s impossible to know for sure. The skin atrophy and other signs can be relatively common with kenalog and other insoluble steroids. I don’t what the “thumb locking” is unless the patient means trigger thumb. Some physicians will use sterile saline injections in the atrophied area to speed up the recovery.