Local anesthetics (anaesthetics) are the most frequently used medication in pain medicine. From numbing up the skin prior to inserting larger needles, to anesthetizing joints and deeper nerves, these drugs are essential for both therapeutic and diagnostic purposes in our daily practice.
MOST COMMONLY USED LOCAL ANESTHETICS
- Lidocaine – Xylocaine (1%, 2%)
- Bupivacaine – Marcaine (0.25%, 0.5%, 0.75%)
- Ropivacaine – Naropin (0.2%, 0.5%, 0.75%, 1%)
MECHANISM OF ACTION
- Block voltage-gated sodium channels, thus blocking signal conduction — “Membrane Stabilizers”
- Remember: A large influx of sodium ions through sodium channels is needed to depolarize a nerve cell membrane and allow for saltatory conduction of the action potential up/down the neuron
WORKS BEST ON SMALL-DIAMETER NEURONS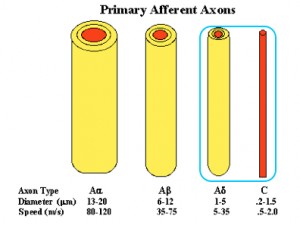
- Aα (alpha) – proprioception (muscle sense)
- Aβ (beta) – touch, pressure, vibration
- Aδ (delta) – fast pain, cold
- C – slow pain, warmth and itch
ESTERS vs AMIDES
- Esters (cocaine, procaine / novocaine)
- Risk of severe allergic reactions secondary to the breakdown product paraaminobenzoic acid (PABA)
- Amides (lidocaine, bupivacaine, ropivacaine) [Hint: the ones with two I‘s are amIdes]
- Much less common allergic reactions
ADDING EPINEPHRINE
- Epinephrine is added to local anaesthetics (LAs) to decrease vascular absorption, allowing for longer anesthetic effect
- About 50% prolonged duration of action
BUFFERING WITH SODIUM BICARBONATE
- The burning sensation of lidocaine being injected into the patient’s skin may quite possibly be the most painful aspect of the injection process.
- Lidocaine is more acidic than human tissue, and this is believed to be the reason for the burning sensation.
- Bicarbonate neutralizes the acidic lidocaine –> Less pain, Faster onset
- Directions
- Add 1-ml of 8.4% sodium bicarbonate to a 10ml bottle of lidocaine (with or without epinephrine) – 10:1 ratio
- Note: the buffered lidocaine decreases the effectiveness of the epinephrine. But since we rarely use epinephrine with our injections in pain medicine, this is less relevant to us.
- The buffered lidocaine has also been shown to have even more antibacterial activity
OTHER WAYS TO TAKE THE STING OUT OF INJECTING LOCAL ANESTHETICS
- Warming the lidocaine and injecting it slowly
- Body temperature lidocaine produces less pain than room temperature
- One study found that the rate of administration of lidocaine had a greater impact on the perceived pain of lidocaine infiltration than did buffering.
COMPARISON OF LOCAL ANESTHETICS (click the chart to the right to enlarge)
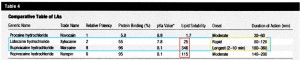
- Quickest onset = Lidocaine
- Least ionized, therefore quickest to pass through tissue and anesthetize the neurons
- Longest duration = Bupivacaine(3-6 hours)
- Because the most protein-bound and fat soluble
- Ropivacaine is in-between lidocaine and bupivacaine with regards to onset and duration — though it costs MUCH more
CONTRAINDICATIONS
- True anaphylactic allergy with AMIDES is extremely rare
- Local sepsis and coagulopathy are relative contraindications
- Intraarticular hemorrhage risk is very low
MAXIMUM SAFE DOSES
- The maximum doses are NOT evidence-based
- The levels are meant to prevent a toxic dose
- Lidocaine
- 30ml of 1% or 15ml of 2% (based on 3mg per kg of body weight)
- Can increase this if using epinephrine
- Bupivacaine
- 25ml of 0.5% or 50ml of 0.25%
- As this all depends on vascular absorption, these numbers will be higher if injected into areas with less vascular uptake (subcutaneously, brachial plexus, epidural)
CENTRAL NERVOUS SYSTEM (CNS) and CARDIAC TOXICITY
- CNS is more sensitive to the effects of LAs, so it is the first to demonstrate an intravascular injection
- CNS toxicity signs:
- Tingling tongue/lips, lightheadedness, shivering, tinnitus, slurred speech, muscle twitching, loss of consciousness, coma, respiratory arrest
- MUCH more sensitive to bupivacaine
- Cardiac toxicity signs:
- Myocardial depression, arrhythmias, ventricular arrest
- Bupivacaine is much more cardiotoxic
- Treating CNS and cardiac toxicities
- IV administered lipid emulsion (LE) has been shown effective in local anesthetic toxicity
SKELETAL MUSCLE TOXICITY
- Seen in experimental settings
- Bupivacaine seems to induce myocyte apoptosis
- Only a few case reports exist, and this is with large amounts such as with continuous peripheral blockade or infiltration of a wound.
- Very rare in the clinical setting
ARTICULAR CARTILAGE / CHONDROCYTE TOXICITY
- At high doses (30-60ml), bupivacaine and all epinephrine-containing LA formulationsdemonstrate increased chondrocyte apoptosis
- Note: with doses in pain medicine being typically 3-10 ml, these chondrocytic doses aren’t relevant to our practices
- Dilutional effects of joint fluid and active absorption
- Intraarticular injections of LAs are unlikely to expose the chondrocytes to the concentrations used for in vitro experiments, because of the dilutional effect of the joint fluid and the active systemic absorption
CLOSING THOUGHTS
- Bupivacaine is the Triamcinolone of local anesthetics — see the “Corticosteroids in Pain Medicine” post for an explanation of this


















I have found a lot of information here that I think might be helpful in talking to a doctor but I am not even sure which doctor I should be talking to. I had a fasciotomy done on my right leg to correct damage caused by compartment syndrome and as a result ended up with severe nerve damage. I have pain, all day, everyday, any time of day! I have learnt to tolerate the allowable numbers on a pain scale and the days I have a 10 kind of pain, that is a good day. I believe that there has to be a solution to the nerve pain I am having because it have really changed my life horribly. I schedule my life around what is the cost capital in pain associated with that activity.
I am trying to figure out is compounded medication and or site anesthetic injections may be able to help, but I have no idea where to start. Any help I could receive would be greatly appreciated. Thank you for your time and attention. God bless you!
That type of situation could have caused complex regional pain syndrome (CRPS). Topical compounded creams may be helped. Desensitization therapy with physical therapy may be helpful. Local injections of anesthetics won’t help. Lumbar sympathetic nerve blocks may help. As a last resort, a spinal cord stimulator implant may be greatly helpful. Find an interventional pain physician that does these to speak to them about it.