By Chris Faubel, MD —
Indications
- Osteoarthritis of the knee
- Knee pain
- Rheumatoid arthritis of the knee
- Gout (in the knee)
- Calcium pyrophosphate dyhydrate (CPPD)
- **see all ICD-10 codes at end of post
CPT code: 20610 “Arthrocentesis, aspiration and/or injection; major joint or bursa”
Materials Needed
- Pen – clicking type
- Gloves – non-sterile
- Alcohol swabs (or providone-iodine)
- Band-aid
- 25-gauge 1.5″ needle (depending on body habitus) and 3-5ml syringe
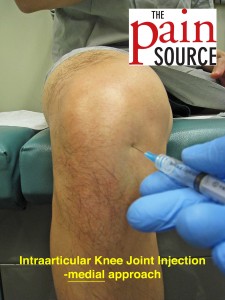
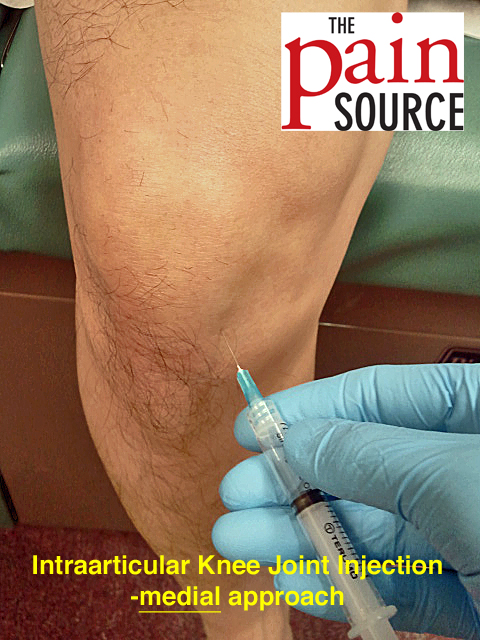
Medial Approach. Advance needle at about 15-20 degrees from midline. - Injectate
- 1-ml of 40mg/ml Depo-Medrol or Kenalog
- 2-4ml of 1% lidocaine
- For skin numbing: Tuberculin needle/syringe (27-gauge, 1/2″) filled with 1ml of 1% lidocaine
Technique / Procedure Steps
- Always start with informed consent from the patient, and then a time-out to verify correct patient and injection site.
- Mark the injection site with the pen tip in order to leave an impression in the skin.
- Clean the skin thoroughly with as many alcohol swabs as needed (usually 1-2 is needed).
- Patient position: seated (legs off the side of the table/chair)
- With the 25G 1.5″ needle, enter the skin going obliquely (roughly 15-20 degrees from midline) into the joint. If any periosteum is met with the needle tip, redirect. Typically need to use all of the 1.5″ needle.
- Aspirate to make sure you’re not in any vessel.
- After negative aspiration, inject the full contents of the syringe. Redirect or withdraw the needle slightly if it isn’t flowing easily.
- Withdraw the needle and apply band-aid.
Tips
- Finding the injection site
-
- Palpate the patellar tendon, and then fall off either the medial or lateral side. That depression (dimple) is your injection site.
-
- Patients typically have more medial compartment narrowing, so I tend to access the knee into the lateral compartment.
- Numbing the skin
- Find out all about “Taking the Sting Out” (of injections) by going here.
- Since I use a 25G needle, most patients have no problem with the injection and don’t need any extra lidocaine skin wheal or freezing spray.
- I tell them numbing the skin with lidocaine may possibly hurt more than the actual injection.
- Procedure for a “pain free” injection
- Fill a 27G 1/2″ tuberculin syringe with 1-ml of 1% lidocaine.
- Use ethyl chloride spray to “numb” the skin over the injection site; then quickly create the skin wheal of lidocaine.
- Insert the tip of the needle just below the surface of the skin, almost at a parallel angle. Then inject about 0.25-ml to create the skin wheal.
- Redirect the needle perpendicular to the skin in the direction that your 25G needle will go, and inject the rest of the Tb syringe along the entire length of the needle.
- After the injection
- Have the patient move their knee for a few seconds while you throw away used supplies.
- Then, have the patient stand and walk around so they can see the immediate results of the lidocaine.
- Explain to the patient that the lidocaine will wear off in an hour or so, and that they will be back to their normal pain until the steroids start kicking in (anywhere from 1-7 days).
- May also ask the patient to not do much activity with that knee for 12-24 hours.
ICD-10 Diagnostic Codes
- Osteoarthritis of the knee
- M17.31 “unilateral post-traumatic osteoarthritis, right knee”
- M17.32 “unilateral post-traumatic osteoarthritis, left knee”
- M17.11 “unilateral primary osteoarthritis, right knee”
- M17.12 “unilateral primary osteoarthritis, left knee”
- M17.2 “bilateral post-traumatic osteoarthritis of knee”
- M17.0 “bilateral primary osteoarthritis of knee”
- Knee Pain
- M25.561 – right knee pain
- M25.562 – left knee pain
- Rheumatoid arthritis of the knee
- M05.661 “rheumatoid arthritis of right knee WITH involvement of other organs and systems”
- M05.662 “rheumatoid arthritis of left knee WITH involvement of other organs and systems”
- M05.761 “rheumatoid arthritis with rheumatoid factor of right knee WITHOUT organ or systems involvemen”
- M05.762 “rheumatoid arthritis with rheumatoid factor of left knee WITHOUT organ or systems involvement”
- Gout in the knee
- M10.062 “idiopathic gout, left knee”
- M10.061 “idiopathic gout, right knee”
- M1a.062 “idiopathic chronic gout, left knee”
- M1a.061 “idiopathic chronic gout, right knee”
- Calcium pyrophosphate dehydrate (CPPD) of the knee
- M11.251 “other chondrocalcinosis, right hip”
- M11.252 “other chondrocalcinosis, left hip”














Very good site for learning injection techniques.
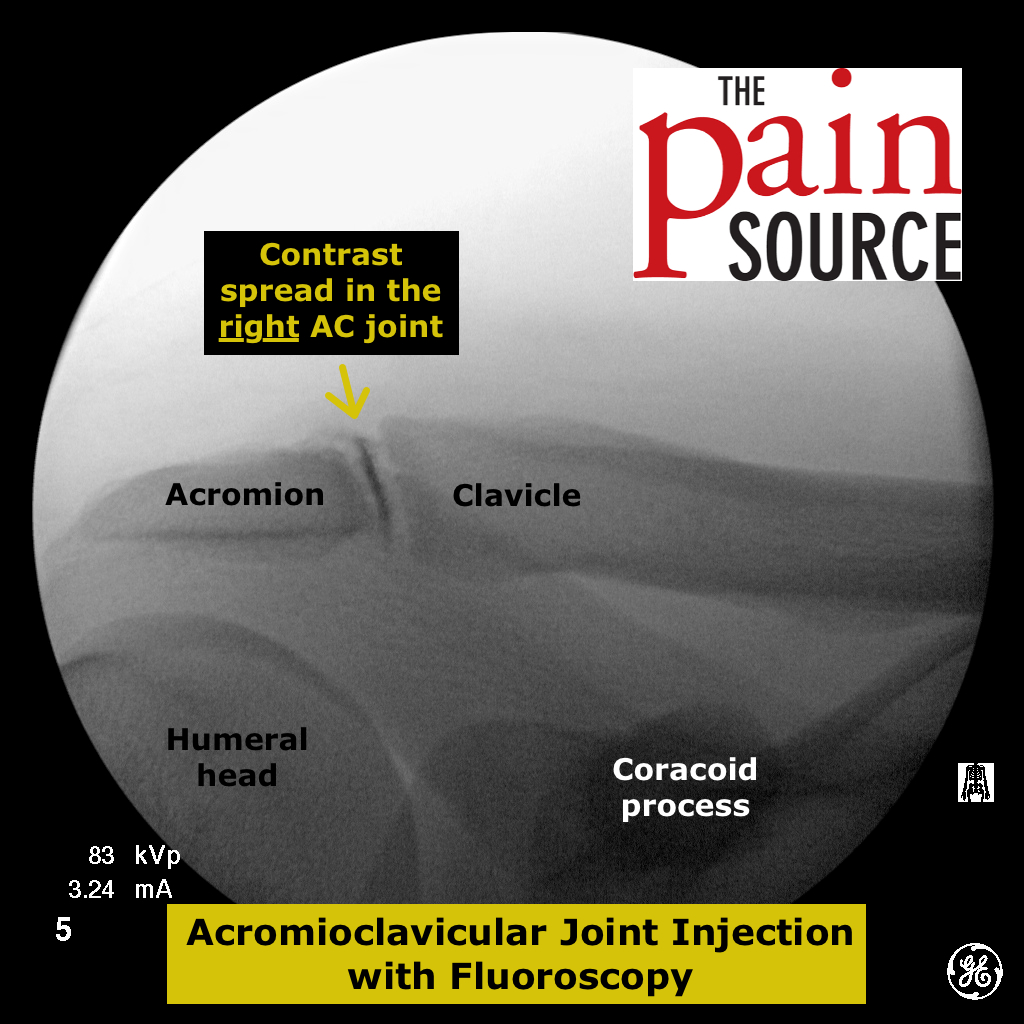
I notice an error in the knee injection tips. It talks about the acromion and clavicle which is obviously from the shoulder injection tips section
Thanks a lot for pointing out that mistake.
Hi Doctor,
I had a cortisone shot in my left knee yesterday ( more than 24hrs).
I wasn’t in severe pain but the doctor recommended because I have patellofemoral syndrome ( ostheoarthritis +50). After the shot I have been in severe pain not being able to stand up or straight the leg or bend it without pain. I called the doctor and he doesn’t work today. This was suppose to help me and I am back to the pain when I partially dislocated my knee.
Is this normal after a cortisone shot? I am writting you because it is the only webpage that I found with the same tecnique that my doctor use (inside,infront of my knee).
I hope you can help me with feedback about my horrible pain (specially behind my knee) or any other explanation of why this is happening.
Thanks so much!!
Another question is it the same patellofemoral syndrome than ostheoarthritis?? The only difference is for young people doctors refer as PFemoral Syndrome and for older patiens OA???? Thanks and God bless you.
Pain after a corticosteroid injection is not the norm, but it’s not abnormal either. I can’t speak to your situation, but I can say that occasionally patients will have what’s called “post injection flare” where the pain is worse for 2-3 days after the injection. I would tell patients to put ice on the area and as long as it’s not red, swollen or with discharge at the injection site, sit on it for a couple days to see if it resolves. If it’s not any better after 2-3 days, then come into the office. And just so you know, it does NOT mean the injection did or did not work correctly, and it does not matter which technique was used to get the steroid into the knee joint.
Nice
Just wondering if you could use a 27 gauge for intraarticular knee injections and what your thought process was on utilizing smaller gauges and how you decide which gauge to use, thanks for the education and well designed articles!
They don’t make a 27-gauge long enough with this approach to the knee. It would also make injecting the steroid solution very difficult. You want to feel the solution go into the knee joint with ease. You don’t want there to be resistance to the flow of the solution out of the needle tip. If you get that resistance, you may be inside a ligament, and you don’t want to be injecting it there. So skip the 27-gauge and go for a 25-gauge, and many times I’ll use a 22-gauge 3.5″ Quincke needle.
Hi Doctor,
Question for you on diagnosis codes for knee OA: historically (before ICD10) when would 719.46 “pain in joint, lower leg” be used instead of the OA-specific codes (i.e. the 715.xx branch)? I’m curious why the 719.46 code would be used if OA were the diagnosis.
Also, in ICD10, I believe there is a corresponding equivalent for 719.46: code M25.569. Would you include that in OAK diagnosis?
Thanks very much!
Knee Pain
M25.561 – right knee pain
M25.562 – left knee pain
“Knee pain” is just a more general code to use when you don’t have confirmed OA