Before getting CT or MRI with IV contrast
- Serum BUN and creatinine (within 72 hours of test)
- Note: If patient is taking glucophage-containing medications, let the radiology department determine whether to hold it for 48 hours after giving the IV contrast.
Osteoporosis
- CBC, CMP, TSH, vitamin D (25-hydroxyvitamin D)
- Serum calcium, phosphate, and alkaline phosphatase levels are normal in primary osteoporosis
- Many other diagnostic tests for secondary osteoporosis here: Medscape article
- DEXA scan: T-score -1 to -2.5 = osteopenia; >-2.5 = osteoporosis; Medscape article
Fibromyalgia vs Myopathy
- In order to rule out a true myopathy or myositis that could explain the muscle pain in a suspected fibromyalgia patient, some lab tests may be needed.
- First, see if the patient is on a statin medication (is there a rough temporal relationship between when they started the statin and when the symptoms began?).
- Creatine kinase (CK – the single most important diagnostic test) and Vitamin D (25-hydroxyvitamin D) to start with. If positive, you can also order AST (SGOT), ALT (SGPT), LDH, GGT, aldolase,
- Nerve conduction studies will be normal in patients with myopathy and fibromyalgia alone.
- Needle EMG will be normal in fibromyalgia, but in myopathy will show small amplitude motor units with increased (early) recruitment; keep in mind that EMG may be normal in patients with myopathy too (look at the whole picture).
- If myopathy is suspected at this point, refer to a neurologist or rheumatologist. A muscle biopsy may be needed.
Psoas Abscess (suspected)
- CT of abdomen and pelvis with IV contrast
Spinal metastasis (suspected)
- MRI with and without IV contrast
Discitis (suspected)
- CBC, ESR, CRP
- MRI with contrast
Vertebral Compression Fracture (suspected)
- MRI with STIR sequences (STIR suppresses the fat signal in the vertebral body and just shows the white signal of edema from an acute or subacute fracture)
Hardware Failure (Pedicle Screw Fracture)
- CT with reconstruction
Seronegative spondyloarthropathies (AS, reactive, psoriatic, inflammatory bowel-associated)
- Ankylosing spondylitis has clinical findings similar to facet arthritic pain (worse in the morning, improves with activity, nocturnal component), though it is MUCH less common.
- Labs (all are non-specific): rheumatoid factor, HLA-B27, CRP, sed rate
- Radiographs: AP X-ray of bilateral sacroiliac joints (AP pelvis) and AP/lateral lumbar spine
Vascular claudication (suspected)
- Order an ankle-brachial index (ABI)
- If <0.9, consider getting an aortogram with runoff; or just refer to a cardiologist or vascular surgeon

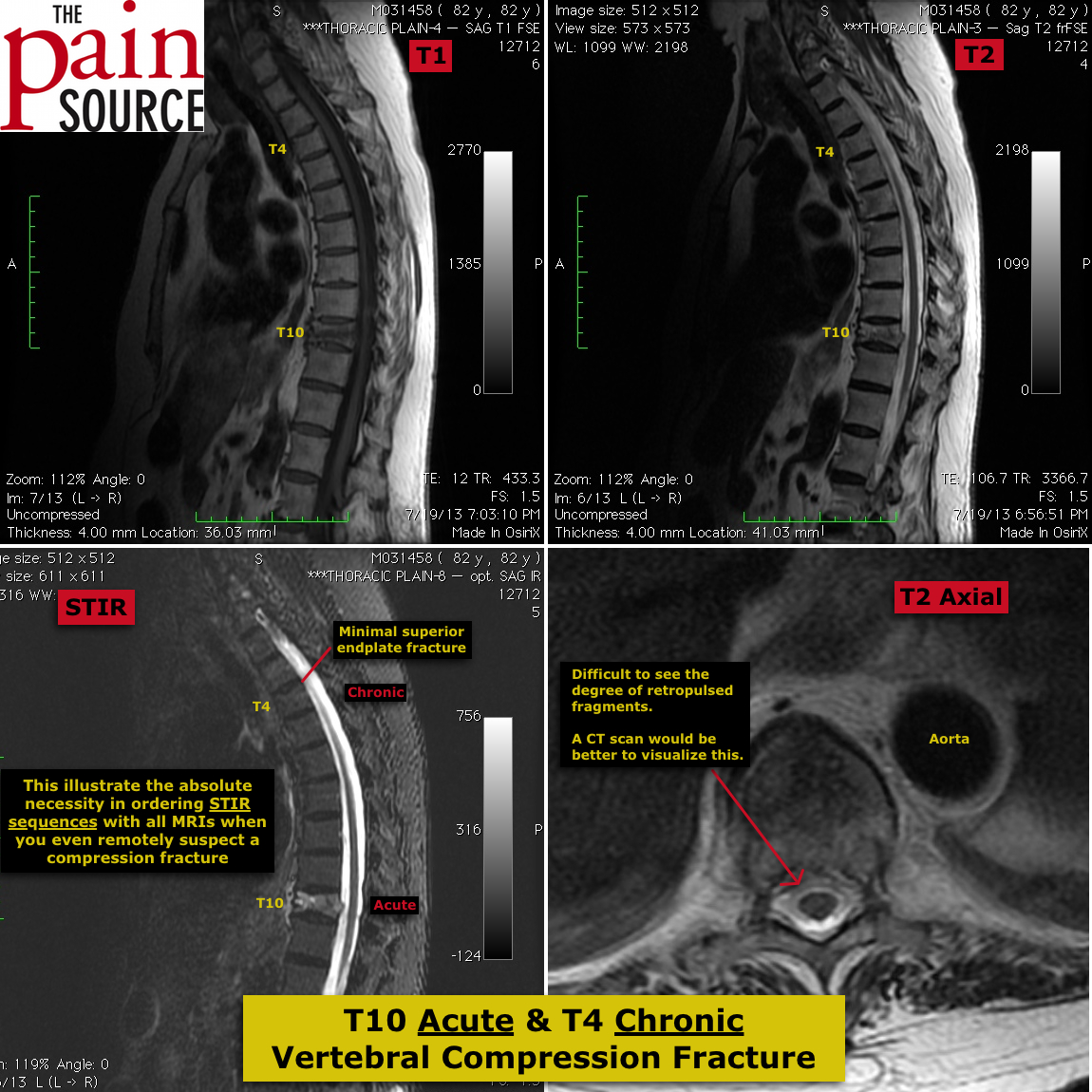














I’m very glad you emphasized a STIR sequence on MRI evaluation for a vertebral compression fracture. That sequence will be most sensitive for edema which will correlate well with response to Kyphoplasty. However, it should be known to avoid open MRI’s for this evaluation as most open MRI’s cannot do STIR sequences or even T2 fat saturation sequences well. It also helps to request the spine MRI be read by a musculoskeletal or neuroradiologist who has examined the pt to correlate with site of pain. If the patient cannot have an MRI (pacemaker, stim, dangerous metal, or severe claustrophobia) evaluation can be performed with a CT and bone scan. Any comparison images can be reviewed to demonstrate progression of fracture.
Thanks a lot it is really excellent site very useful .