By Chris Faubel, MD —
Patients undergoing transforaminal epidural steroid injections show greater functional improvement if they have positive EMG findings of lumbar radiculopathy.
J Pain. 2008 Jan;9(1):64-70.

The use of electromyography to predict functional outcome following transforaminal epidural spinal injections for lumbar radiculopathy.
Fish DE, Shirazi EP, Pham Q.
Department of Orthopedics, UCLA School of Medicine, Los Angeles, California 90404
Get the abstract here
Summary of Study
- Purpose: to determine if objective EMG findings can predict functional benefit after a lumbar transforaminal epidural steroid injection
- Retrospective chart review
- Study Participants
- Patients who presented to the Veterans Affairs (VA) hospital in Los Angeles between July 1, 2000, and June 30, 2002.
- Pain level and functional status (using the Oswestry Disability Index – ODI) was filled out before the injection, and at a follow-up visit (and these were kept electronically).
- Inclusion criteria
- EMG completion before the procedure with a diagnosis of an L5 or S1 radiculopathy
- Transforaminal epidural steroid injection (TF-ESI) performed at L4 and/or L5
- Symptomatic pain in only one extremity
- Completion of self-assessment surveys before the interventional spine procedure and at follow-up
- To be considered “EMG-positive”
- Evidence of denervation or reinnervation on needle EMG
- Two muscles innervated by 2 nerves from the same spinal cord level needed to be positive .
- Baseline characteristics
- Number of patients = 39
- Age = 60 (mean; ± 12.5 years)
- Methods
- The level of injection was based on the EMG findings, physical examination, magnetic resonance imaging (MRI), and clinical symptoms.
- No patient received more than two levels of injections.
- Injectate used
- 40-mg triamcinolone acetonide (Kenalog) + an unknown amount of 1% lidocaine
- If two levels were injected, the injectate was divided equally between the two levels.
- Results
- The pre-injection ODI (Oswestry Disability Index) scores were essentially equal.
- The pre-injection pain scores on the VAS were similar as well.
- Two groups
- EMG-positive patients
- 18 patients
- Post-injection ODI improvement = 7.11
- EMG-negative/normal patients
- 21 patients
- Post-injection ODI improvement = 3.2
- EMG-positive patients
- The post-injection VAS scores were improved after the injection, but the difference between the groups was not statistically different.
- Limitations of the study
- No evaluation of medications taken or changed during the pre- and post-injection ODI
- No comparison of prior surgical interventions to the lumbar spine
- No standardized time between symptom onset and EMG testing
- Not a heterogenous group of patients
- The injectionists were not blinded to the EMG results
- Conclusion
- Patients undergoing transforaminal epidural steroid injections show greater functional improvement if they have positive EMG findings of lumbar radiculopathy.
- Analog pain scores do not help in the decision-making of treatment options for patients with lumbar radiculopathy.
- This study shows the diagnostic value of needle EMG in the prognostic success of patients prior to lumbar TF-ESIs, while simple pain scores are of little value.
Future Research
- Evaluate the psychological and medication factors that may determine a patient’s relief from lumbar epidural steroid injections.
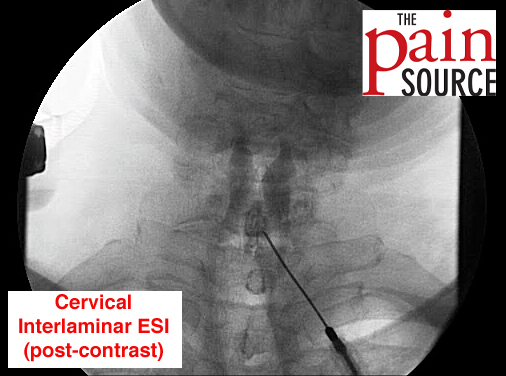
- Also look at interlaminar vs transforaminal ESI relief in EMG-positive vs EMG-negative patients.








Hello, my name is Rachael I’m 36 and I’ve suffered from chronic sciatica for almost 10yrs now. We think it’s due to a car accident at 19yrs old and pregnancy. Over the past year Iv e had a series of injections…4lumbar, si joint, nerve blocker, racet injection and rhizotomy, some worked better than others but not any longer than a couple weeks. Also, my emg says radiculopothy at l4 l5 and s1 but I have no significant bulging or herniated disc. I do show arthritis as well as facet arthropathy. The last lumbar epidural seems to lasting and gave me more relief than any others. So I’d say my pain decreased about 50% and it’s been about 2months now. The pinching around my si joint area is better too. I have pain in my whole lose back and numbness, I have groin, hip, buttocks, thigh, calf, knee and foot pain. I have numbness and needles in my foot and thigh on a daily basis. Also I’ve seem 3 neurosurgeons who say I have nerve damage and there isn t anything the can due surgically so back to pain management I go. In my experience it won t be long before all the pain comes back. My pain management doc wants me to get another emg (8 months ago emg showed moderate radiculopothy l4, l5, s1) my question is…will my new emg (scheduled next week) still show radiculopothy even though I just had lumbar epidural 2 months and pain not back completely? I guess I’m asking..does lumbar epidural sure radiculopothy not caused but disc issue or does epidural just mask the pain? Thank you and sorry, I tried to make as much sense as possible. My doctor is being gauge and my guess is waiting for new emg, but could it have drastically changed in 8 months?
Relief from an epidural steroid injection but continued numbness/tingling will still show nerve damage on the EMG/NCS if it exists. Also, epidural steroid injections treat the pain by getting rid of the inflammation; they don’t block or mask the pain. Good luck.