By Chris Faubel, MD —
Case Presentation:
A 39-year-old right-handed hair dresser presents with a 3-month history of severe right upper extremity pain (radiating down the posterior arm, forearm, and into the middle finger). She has received conservative management with medications and physical therapy, but the severe pain continues to adversely affect her functional status (unable to perform many ADLs and cut hair at work).
Physical exam revealed 5/5 MMT of the bilateral upper extremities, but with decreased sensation over the dorsal aspect of the right middle finger. Decreased right triceps reflex compared to the left. Negative Hoffman’s. No ankle clonus or hyperreflexia. Spurling’s test was positive on the right.
Plan: Perform a cervical transforaminal epidural steroid injection (C-TFESI).
Questions: What type of corticosteroid should be used? What should you know about the cervical anatomy and risk of performing a cervical transforaminal ESI?
Introduction
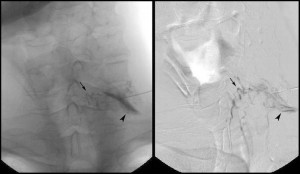
Cervical epidural steroid injections (C-ESIs) are particularly effective in the treatment of cervical radiculopathy [13]. The transforaminal approach is preferred over the interlaminar approach when particular nerve roots are desired to be targeted. Because of this, cervical transforaminal epidural steroid injections (C-TFESIs) are often referred to as “cervical selective nerve root injections/blocks” — although some research has shown the injections aren’t as specific to just one level, as once believed.
Many neurosurgeons will request specific nerve roots blocked for diagnostic purposes when deciding whether to proceed with surgery.
The fear of spinal cord and brain infarctions has caused many pain medicine practitioners to abandon the transforaminal approach for cervical epidural steroid injections. The perceived, relative safety of the interlaminar approach has led to its preference when corticosteroids in the cervical epidural space are deemed beneficial for the patient. Here, I will present the appropriate anatomy and evidence-based knowledge surrounding this transforaminal approach, the associated risks, and finally, methods to minimize those risks.
Anatomy of the Cervical Spine
No injection should be performed without first knowing the anatomy of the area being injected. This is especially true when using the transforaminal approach for cervical epidural steroid injections.
- Comparison with Lumbar Spine
Source: eOrthopod - More forward angling of the transforaminal space (exit of nerve root)
- Large transverse foramen with the vertebral artery (not shown in eOrthopod picture to right)
- Presence of the spinal cord
- Intervertebral Foramen (Cervical)
- The cervical nerve root exits the inferior part of the foramen, just above the correspondingly numbered vertebral body (example: the C7 nerve root exits above the C7 vertebra).
- Vertebral arteries traverse through the foramina in the transverse processes (transverse foramen) and reside in the anterior aspect of the intervertebral foramen.
- Radiculomedullary branches from the vertebral arteries and other cervical arteries (deep cervical and ascending cervical arteries) traverse the anterior foramen as well.
- As you will see below, this anterior placement of the radicular arteries is not 100%.
- Vascular Anatomy – Spinal Cord
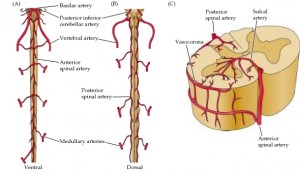
Source: ncbi.nlm.nih.gov - The anterior 2/3 of the spinal cord is supplied by the ONE anterior spinal artery, with the posterior 1/3 supplied by the TWO posterior spinal arteries.
- Anterior Spinal Artery
- Arises from the coalescence of the two vertebral arteries.
- Supplied along the cord length by segmental radicular arteries (including the artery of Adamkiewicz near the lower thoracic spine) every 3-5 vertebral segments
- Watershed areas are created by this segmental vascular supply, and this allows for areas of the cord to be particularly sensitive to ischemia.
- Posterior Spinal Artery
- Arises from the vertebral arteries and the posterior inferior cerebellar arteries (PICA)
- Also receives segmental supply from the radicular arteries
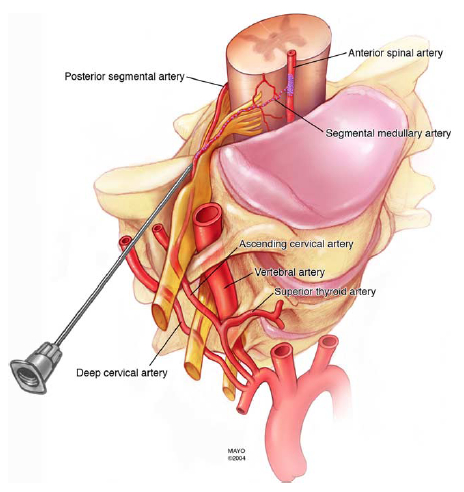
- Vascular Anatomy – Cervical Spine
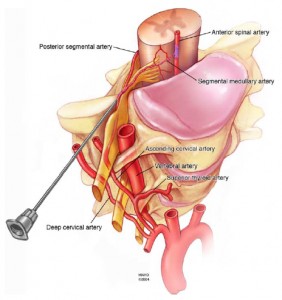
Source: Mayo Foundation for Medical Education and Research - Vertebral arteries
- Arise from the subclavian arteries, enter the transverse foramen at the C6 level, and travels superiorly to the C1 level (atlas).
- Cervical radicular arteries
- Previously thought to reside exclusively in the anterior aspect of the intervertebral foramen, and therefore, the posterior foramen was the “safe” target for the needle.
- A recent cadaveric study by Huntoon [3] shed light on the variability of the vasculature traversing the cervical intervertebral foramina.
- Of the 95 foramina dissected, seven (7) had spinal branches in the posterior foramen, potentially forming radicular or segmental medullary vessels to the spinal cord.
- Of the seven spinal branches above, three were included in deep dissections, and in fact DID contribute to segmental medullary arteries and radicular arteries.
- One additional ascending cervical artery formed a segmental medullary artery that joined the anterior spinal artery.

- 3 – Huntoon MA. “Anatomy of the cervical intervertebral foramina: vulnerable arteries and ischemic neurologic injuries after transforaminal epidural injections”. PAIN. 117, 2005; 104-111
- Of the 95 foramina dissected, seven (7) had spinal branches in the posterior foramen, potentially forming radicular or segmental medullary vessels to the spinal cord.
- Vertebral arteries















Impressive!