By Chris Faubel, MD
J Rheumatol. 2004 Nov;31(11):2265-8.

Intraarticular corticosteroid injection: pain relief in osteoarthritis of the hip?
Kullenberg B, Runesson R, Tuvhag R, Olsson C, Resch S.
Department of Orthopedics, Blekinge Hospital, Karlshamn, Sweden. bjorn.kullenberg@lthlekinge.se
http://www.ncbi.nlm.nih.gov/pubmed
ABSTRACT
OBJECTIVE: Osteoarthritis (OA) is one of the most common causes of morbidity in the elderly population, and surgery is often preceded by years of pain and disability. Intraarticular corticosteroid injections in osteoarthritic joints may play a role in the therapeutic plan and can afford quick pain relief but do not alter the underlying disease. There is a paucity of well controlled studies that provide recommendations for the use of corticosteroids in OA of the hip.
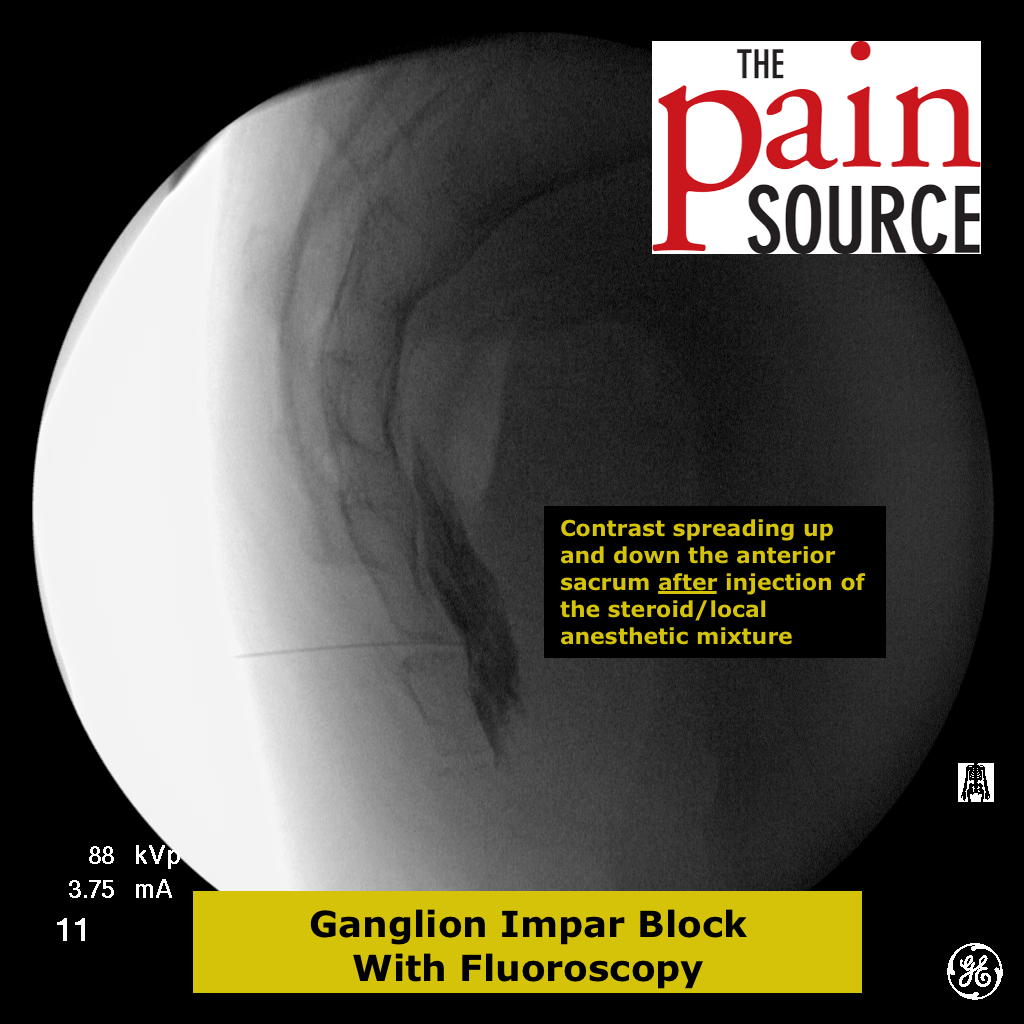
METHODS: A prospective analysis of 80 patients with OA of the hip and pain at rest and on bearing weight for more than 4 weeks was performed. Patients were randomized into 2 groups; group 1 (n = 40) received corticosteroid (80 mg triamcinolone acetonide) and group 2 (n = 40) local anesthetic (1% mepivacaine), injected into the hip joint under fluoroscopy. Pain, functional ability, range of motion of the joint, and analgesics consumed were registered 3 weeks postinjection. The treatment was blind for the patients and the investigators performing the followup.
RESULTS: Pain for all modalities decreased after corticosteroid injection, but pain at rest decreased the most. There was significant pain reduction at the 3 (and 12) week followup. Joint range of motion increased significantly for all directions. Functional ability improved significantly after injection. We found no significant pain relief or improvement of functional ability in patients treated with local anesthetics.
CONCLUSION: This study suggests that intraarticular corticosteroids might improve pain and range of motion of the affected joint in patients with hip OA.
Great, full-text version of the study can be found for free online here
——————————————————-
SUMMARY / MY THOUGHTS
Kullenberg et al (2004) evaluated the effectiveness of intraarticular corticosteroid injections in eighty (80) patients with hip osteoarthritis and pain for more than 4 weeks.
Inclusion criteria:
- The patients were on the waiting list to get a total hip arthroplasty
- All had hip pain for more than 4 weeks, and a VAS of >3 with ambulation and rest
- Hip osteoarthritis (OA) on x-ray
Two groups:
- Group 1: 40 patients = triamcinolone acetonide (Kenalog) – 2ml (80mg)
- Group 2: 40 patients = mepivacaine (Carbocaine; local anesthetic) – 2ml
- Mean age for group 1 (steroid-only) was 67.3 years, and for group 2 it was 72.7 years
- Pain with VAS (visual analogue scale) before and after the injection
- three (3) and twelve (12) weeks
- Time to pain relief
- Duration of effect
- Changes in function
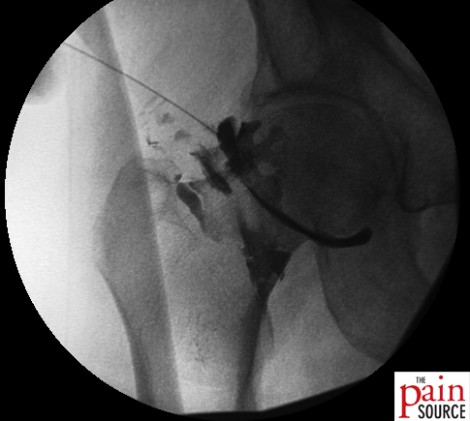
- Anterior approach with a 22-gauge needle under fluoroscopy
- 2ml of mepivacaine and 2ml of 40mg/ml kenalog was used – so each group had the same volume of injectate
- Patients told to rest after the injection. Could resume normal activities the following day.
- No complications in either group
- Steroid group
- Significant decrease in VAS score (especially at rest)
- Increase in hip mobility in all planes, but especially in internal rotation
- Decrease in analgesic intake afterwards
- Before the steroid injection, 22/40 patients used analgesics occasionally and 16/40 daily
- After the steroid injection, 16/40 used them occasionally and 3/40 daily
- Local anesthetic group
- NO significant pain relief
- NO significant improvement in functional ability
- All patients withdrew from the study before 12 weeks due to lack of effect
Important note: Twenty percent (20%) of the patients in the study underwent surgery during the study, with no difference between the groups.