By Chris Faubel, M.D. —
There are two very important things to know about benign hemangiomas in the spine
1. Distinguishing from cancer metastasis to the spine
2. Knowing the sequelae of a benign hemangioma in the spine
Distinguishing from Spinal Metastasis
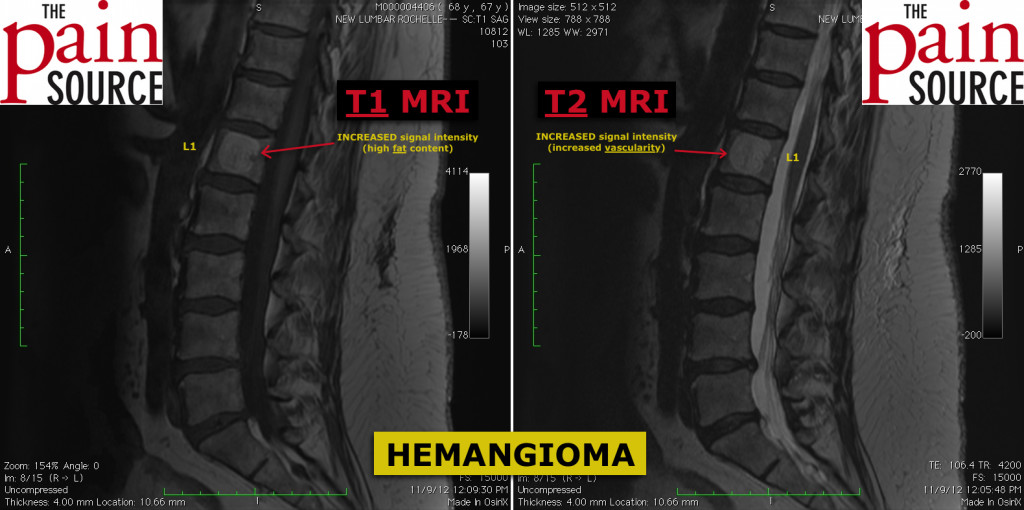
When you look at a patient’s MRI and spot lesions that have an increased signal intensity on T2-weighted images (the most commonly viewed sequences by interventional pain physicians), you may get worried that these could be cancerous, especially if your patient also has a history of prostate / breast / lung / renal / GI cancer.
Before you get too worried, look at the same slices on the T1-weighted images. Both osteoblastic and osteolytic metastatic lesions are typically hypo-intense on both T1 and T2. For more detail, check out this site: http://radiopaedia.org/articles/vertebral-metastases
On the other hand, spinal hemangioma “light up” (hyper-intense) on both T1 and T2.
Hemangioma in the spine are WHITE on both T1 & T2
Sequelae of Benign Hemangioma
Pathologic Fracture: If these vertebral hemangioma get large enough and weaken the vertebral body integrity enough, a pathologic compression fracture can occur. So if a patient has a known large vertebral hemangioma at L1 and develops pain in that area months or years later, suspect a compression fracture and re-image them with an MRI with STIR sequences.
Patient and Location Characteristics
Benign (and usually asymptomatic) lesions located mostly in the lower thoracic or upper lumbar spine. Females > males. Peak incidence in 40’s.
Check out this article from LearningRadiology.com for more information on spinal hemangioma: http://www.learningradiology.com/archives2008/COW%20317-Hemangioma%20spine/hemangiomacorrect.htm
Treatment
Observation (wait and see). If a compression fracture occurs, consider a vertebroplasty or kyphoplasty.