By Chris Faubel, M.D. —
The risk of performing interventional pain injections while a patient is taking anticoagulant blood thinners has been debated for years. Previously, the most cautious guidelines called for holding anticoagulants not only all prescription anti-coagulants, but also over-the-counter NSAIDs, aspirin, and many herbs/vitamins (gingko, fish oil, vitamin E, etc) for varying numbers of days before the procedure.
Within the last few years, the risk of being taken off these blood thinners, even for a few days, has been shown to be more dangerous than keeping patients on them for certain procedures that are not near the spinal cord or nerves.
The below information regarding the cessation or holding of anticoagulants is for NEURAXIAL PROCEDURES. With these procedures, there is a higher risk of epidural hematoma formation if a vein or artery is punctured near the spinal cord.
Neuraxial procedures (and other pain procedures with higher bleeding risk)
- Epidural steroid injections (interlaminar and transforaminal)
- Spinal cord stimulator trials and implants
- Intrathecal pump placement
- Kyphoplasty / vertebroplasty
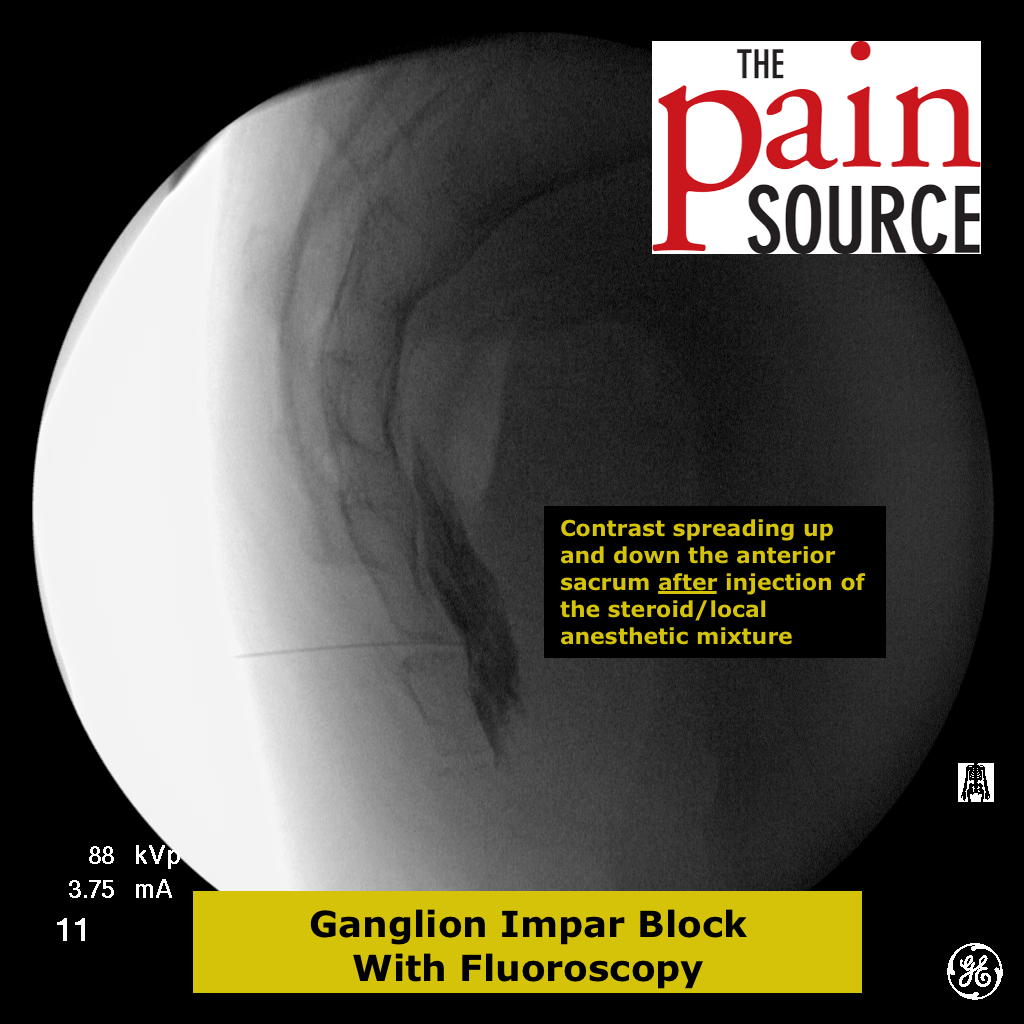
- Sympathetic ganglion blocks
- Cervical and thoracic discograms
Note: It is considered OKAY to continue anticoagulants for other spinal injections/procedures, such as facet (Z-joint) injections, medial branch blocks (MBBs), radiofrequency neurotomy (RFA) and lumbar discograms.
Important: Keep in mind that every patient is different and multiple other variables may apply to the bleeding risk. The below are just guidelines. Also, always get permission from the prescribing physician prior to holding/stopping an anticoagulant.
|
Medication |
Duration to Hold |
Notes
|
| aspirin / NSAIDs |
May Continue |
|
| fish oil, vit. E, gingko, etc. |
May Continue |
|
| warfarin (Coumadin) |
5 days |
INR < 1.3 |
| clopidogrel (Plavix) |
7 days |
Do NOT stop if stent was placed in the past 12 months |
| aspirin/dipyridamole (Aggrenox) |
3 days |
Take a baby ASA those three days |
| dabigatran (Pradaxa) |
2-4 days |
Longer in renal impairment |
| enoxaparin (Lovenox) |
12 hours (prophylaxis) 24 hours (therapeutic) |
Longer in renal impairment |
| heparin |
8 hours (prophylaxis) when aPTT >40s (thera.) |
|
| dalteparin (Fragmin) |
8 hours (prophylaxis) 24 hours (therapeutic) |
Longer in renal impairment |
| fondaparinux (Arixtra) |
48 hours (prophylaxis) 72 hours (therapeutic)
|
Longer in renal impairment |
| rivaroxaban (Xarelto) |
18 hours (prophylaxis) 5 days (therapeutic) |
Longer in renal impairment |
| drotrecogin (Xigris) |
24 hours |
Longer in renal impairment |
| ticagrelor (Brilinta) |
5 days |
|
| abciximab (Reopro) |
48 hours
|
|
| ticlopidine (Ticlid) |
10 days |
|
| apixaban (Eliquis) |
2-3 days |
Longer in renal impairment |
| prasugrel (Effient) |
7 days |
|
| tirofiban (Aggrastat) |
8 hours |
Longer in renal impairment |
| alteplase (TPA) – full dose |
10 days |
Note: Some of the above will not be encountered in an office-based practice because they are only given in a hospital setting.
** The above was collected from the American Society of Regional Anesthesia (ASRA) and the International Spine Intervention Society (ISIS)
Updated August 2013





I am getting a cortisone shot in lower back tomorrow 11-1. I stopped taking xarelto ssunday night. Last dose Saturday night. Cardiologist recommends staying off for three days after injection. What say you?
Waiting 3 days after the injection sounds excessive, but I’d always defer to the cardiologist on this issue.
what about eliqus- how long do you hold before pain injection
2-3 days depending on CrCl. Thanks for pointing out it’s absence.