Disclaimer: The information here is NOT meant to replace the sound advice of a billing and coding expert.
Below is a list of the most common CPT codes (procedure codes) used in a PM&R and interventional pain management clinic. Electrodiagnostic (EMG/NCS) codes are also included. These have all been updated for the most recent 2017 changes. Feel free to make coding tips in the comments below.
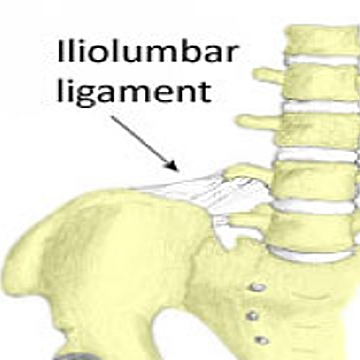
Remember: Use the -50 modifier when performing BILATERAL procedures below. Note: Fluoro needle guidance is built in to SI joint (27096), transforaminal and interlaminar ESIs, medial branch blocks, radiofrequency ablation (RFA) and facet injections; therefore, you can NOT bill for fluoro separately for these procedures. But you CAN bill separate fluoro guidance codes (77002 for non-spinal) for peripheral joints/ligaments/bursa (hips, shoulders, iliolumbar ligament, troch bursa, etc.)
Joints and Bursa – Injection or Aspiration
- Major joint/bursa: 20610 (knee, hip, shoulder, trochanteric bursa, subacromial bursa, pes anserine bursa)
- Intermediate joint/bursa: 20605 (temporomandibular, acromioclavicular, wrist, elbow, ankle, olecranon bursa)
- Minor joint/bursa: 20600 (fingers [PIP, DIP], toes)
- Sacroiliac joint (SIJ) with fluoroscopy: 27096
- Sacroiliac joint (SIJ) without fluoroscopy: 20552 (billed as a trigger point injection)
- Fluoroscopic needle guidance (non-spinal): 77002
- Shoulder arthrogram injection: 23350 (+77002)
- Hip arthrogram injection: 27093 (+77002)
- Genicular nerve blocks: 64450 x3 units
- Genicular nerve RFA: 64640, 64640-59, 64640-59
Tendons, Ligaments, and Muscle Injections
- Tendon sheath or Ligament: 20550 (iliolumbar ligament, trigger finger, De Quervain’s tenosynovitis, plantar fascia)
- Tendon origin/insertion: 20551
- Trigger point injection (1 or 2 muscles): 20552
- Trigger point injection (3 or more muscles): 20553
- Sacroiliac joint (SIJ) without fluoroscopy: 20552 (billed as a trigger point injection)
- Intramuscular injections: 96372
- Fluoroscopic needle guidance (non-spinal): 77002
Nerve Blocks
- Greater occipital nerve block: 64405
- Lesser occipital nerve block: 64450
- Other peripheral nerve: 64450 (I use this for superior cluneal nerve blocks, genicular nerve blocks, and lateral branch blocks for the SI joints)
- Suprascapular nerve: 64418
- Intercostal nerve (single): 64420
- Intercostal nerve (multiple): 64421
- Ilioinguinal and Iliohypogastric nerve: 64425
- Trigeminal nerve (any branch): 64400
- Sphenopalatine ganglion: 64505
- Stellate ganglion (cervical sympathetic): 64510
- Superior hypogastric plexus: 64517
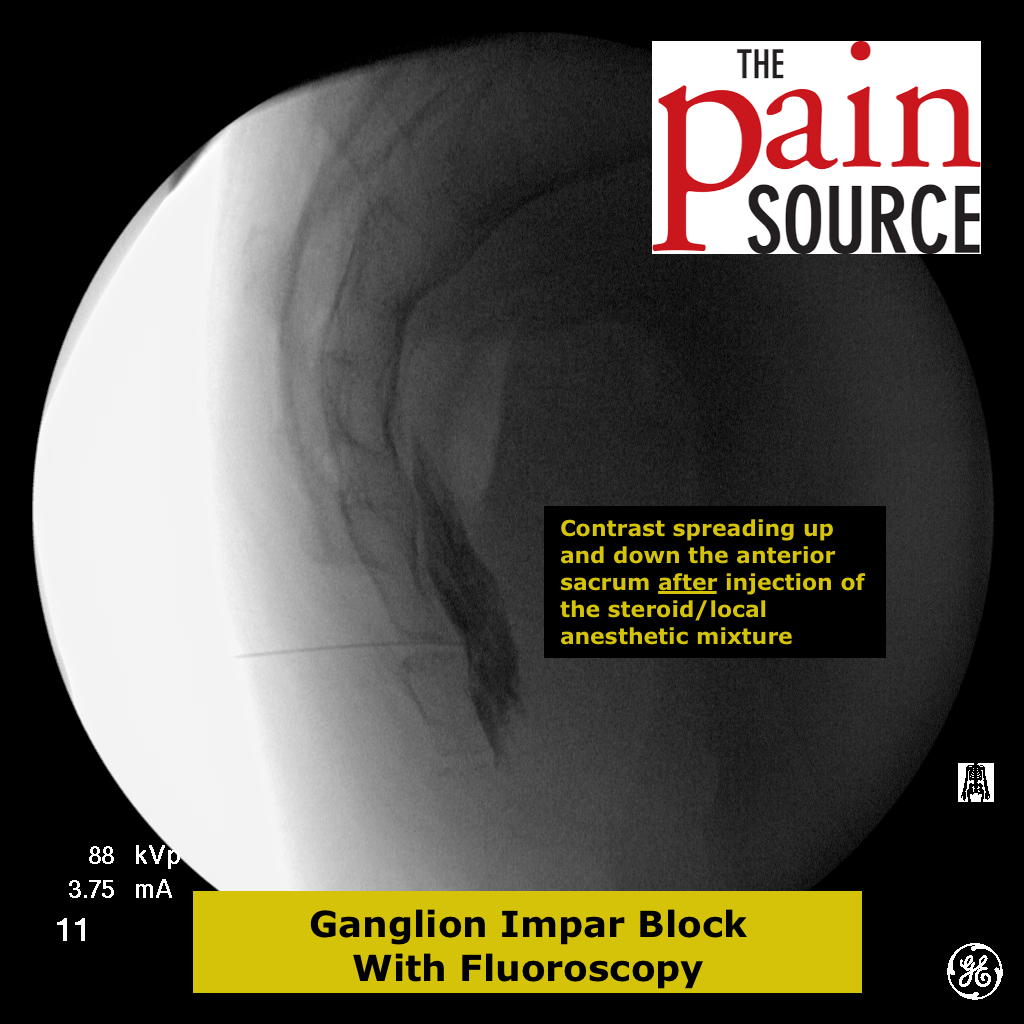
- Thoracic or lumbar paravertebral sympathetic or ganglion impar block: 64520
- Celiac plexus: 64530
- Plantar common digital nerve (Morton’s neuroma): 64455
- Unlisted procedure: 64999
Epidural Steroid Injections (ESI)
-
Interlaminar (WITH fluoroscopic imaging)
- Interlaminar – cervical or thoracic: 62321
- Interlaminar – lumbar or sacral (caudal): 62323
- Remember: Fluoro can NOT be billed separately for these.
-
Transforaminal
- Transforaminal – cervical or thoracic (first level): 64479
- Transforaminal – cervical or thoracic (each additional level): 64480
- Transforaminal – lumbar or sacral (first level): 64483
- Transforaminal – lumbar or sacral (each additional level): 64484
- Remember: Fluoro can NOT be billed separately for these.
- Ex: A bilateral L5 TF ESI would be billed as 64483 -50.
Facet Joint Procedures
-
Intraarticular Joint or Medial Branch Block
- Intraarticular joint or medial branch block (MBB) – cervical or thoracic (1st level): 64490
- Intraarticular joint or medial branch block (MBB) – cervical or thoracic (2nd level): 64491
- Intraarticular joint or medial branch block (MBB) – cervical or thoracic (3rd level): 64492
- Intraarticular joint or medial branch block (MBB) – lumbar or sacral (1st level): 64493
- Intraarticular joint or medial branch block (MBB) – lumbar or sacral (2nd level): 64494
- Intraarticular joint or medial branch block (MBB) – lumbar or sacral (3rd level): 64495
- Note: You can bill for bilateral facets or MBB at the same levels (with the -50 modifier), but you will NOT typically get reimbursed for over 3 facet joints or medial branches on the same side.
- Note: For medial branch blocks, the proper billing is to bill for each complete facet joint blocks (see example below)
- Ex: Bilateral L3, L4, L5 MBBs would be billed as 64493 -50, 64494 -50.
- Note: The third occipital nerve (TON) partially innervates the C2/3 facet joint, so along with a C3 MBB, this would be billed as one full joint (64490)
- Ex: Right TON, C3, C4, C5 blocks = Three full facet joints (C2/3, C3/4, C4/5) = 64490, 64491, 64492
- Remember: Fluoro can NOT be billed separately for these.
-
Radiofrequency Ablation (RFA) / “Destruction” of Facet Joint
- Radiofrequency ablation (RFA) – cervical or thoracic (1st joint): 64633
- Radiofrequency ablation (RFA) – cervical or thoracic (each additional joint): 64634
- Radiofrequency ablation (RFA) – lumbar or sacral (1st joint): 64635
- Radiofrequency ablation (RFA) – lumbar or sacral (each additional joint): 64636
- Remember: Fluoro can NOT be billed separately for these.
Sacroiliac Joint
- Sacroiliac joint (SIJ) without fluoroscopy: 20552 (billed as a trigger point injection)
- Sacroiliac joint (SIJ) with fluoroscopy: 27096
- Sacral lateral branch blocks: 64450 (remember to bill 77003 with these, but not with the 64493 code)
- Radiofrequency Ablation (RFA) of the Sacroiliac Joint
- RF of L5 dorsal primary ramus: 64635
- RF of S1 lateral branches: 64640
- RF of S2 lateral branches: 64640
- RF of S3 lateral branches: 64640
- Fluoroscopic needle guidance (Spinal): 77003 (for the S1-S3 nerve lateral branches, not the L5)
- Note: Use 724.6 (Disorder of the sacrum) and 721.3 (lumbar spondylosis) as the diagnostic codes
Vertebroplasty / Kyphoplasty
-
Vertebroplasty
- Vertebroplasty – Cervicothoracic (1st level): 22510
- Vertebroplasty – Lumbosacral (1st level): 22511
- Vertebroplasty – Each additional level of the above: +22512
- Note: Same charge whether you perform unilateral or bilateral injection of cement (PMMA). Modifier 50 can NOT be used.
- Note: The global charge for the procedure includes all imaging guidance and any bone biopsy performed.
-
Kyphoplasty
- Kyphoplasty – Thoracic (1st level): 22513
- Kyphoplasty – Lumbar (1st level): 22514
- Kyphoplasty – Thoracic or Lumbar (each additional level): +22515
- Note: Same charge whether you perform unilateral or bilateral injection of cement (PMMA). Modifier 50 can NOT be used.
- Note: 10-day global period
Neurostimulation (Spinal Cord Stimulator / Dorsal Column Stimulator)
-
Trial Procedure
- Percutaneous implant of electrode array: 63650 (includes 10-day global) – bill two units if you implant two trial leads
-
Implantation of Spinal Cord Stimulator Percutaneous Leads and Generator
- Percutaneous implant of electrode array: 63650 (includes 10-day global)
- Insertion or replacement of pulse generator: 63685 (includes 10-day global)
-
Implantation of Spinal Cord Stimulator PADDLE Leads and Generator
- Laminectomy for implant of neurostimulator electrode, paddle: 63655 (includes 90-day global)
- Insertion or replacement of pulse generator: 63685 (includes 10-day global)
-
Removal of Leads/Generator (Explant)
- Removal of spinal neurostimulator percutaneous array(s): 63661 (includes 10-day global)
- Removal of spinal neurostimulator paddle electrode: 63662 (includes 90-day global)
- Removal of pulse generator: 63688 (includes 10-day global)
- Important: Also bill for the implanted neurostimulator electrodes (each lead): L8680
Discogram / Discography
- Discogram / Discography – Cervical/Thoracic (each disc): 62291
- Supervision & interpretation of fluoroscopy – Cervical/Thoracic (each disc): 72285
- Discogram / Discography – Lumbar (each disc): 62290
- Supervision & interpretation of fluoroscopy – Lumbar (each disc): 72295
- Remember: Fluoroscopy is bundled here and can NOT be billed separately for these.
Botulinum Toxin Injections
- Botulinum toxin type A – Botox, Dysport (per unit): J0585
- Botulinum toxin type B – Myobloc (per 100 units): J0587
- Needle electromyography in conjunction with chemodenervation: 95874
- Chemodenervation of muscles in the neck (spasmodic torticollis): 64616
- Chemodenervation of muscles of the trunk and/or extremity (cerebral palsy, dystonia, multiple sclerosis): 64614
- Chemodenervation of muscles innervated by facial, trigeminal, cervical spinal and accessory nerves, bilateral (chronic migraine): 64615
Other
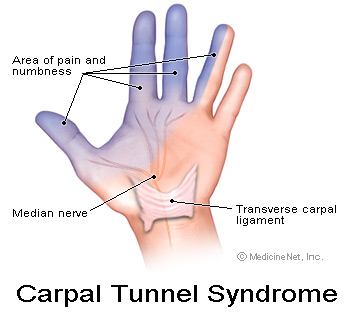
- Carpal tunnel injection: 20526
- Epidural blood patch: 62273
- Moderate sedation (first 30 minutes): 99144 (requires presence of another trained person to monitor the patient’s consciousness and vitals)
- Moderate sedation (each additional 15 minutes): 99145
- Fluoroscopic needle guidance (spinal): 77003
- Fluoroscopic needle guidance (non-spinal): 77002
- CT needle guidance: 77012
Acupuncture
- with electrical stimulation: 97813
- without electric stimulation: 97810
Modalities
- Diathermy (Microwave): 97024
- Heating pads / cold packs: 97010
- Self-care / home management training: 97535
- Therapeutic ultrasound: 97035
- Traction: 97012
- Transcutaneous Electrical Nerve Stimulation (TENS): G0283
Osteopathic Manipulative Treatment
- OMT 1-2 body regions: 98925
- OMT 3-4 body regions: 98926
- OMT 5-6 body regions: 98927
- OMT 7-8 body regions: 98928
- OMT 9-10 body regions: 98929
(note from a reader: use 98928 or less if OMT done in conjunction with an injection and 98927 or less of OMT done in conjunction with epidural)
Modifiers
- -50: Bilateral
- -52: Incomplete procedure (reduced service) [Stopping a part of a procedure because of reasons other than the patient’s well-being]
- -53: Incomplete procedure (physician elected to terminate a surgical or diagnostic procedure due to the patient’s well-being) – reduced service. I’ve used for a patient that had a severe vasovagal response to a radiofrequency procedure and I elected to abort the procedure and reschedule later.
- -59: Indicates that a procedure or service is separate and independent from other services performed the same day
- -26: Professional component only
Injectables (J-codes)
- Omnipaque 300 (per ml): Q9967
- Omnipaque 240 (per ml): Q9966
- Dexamethasone sodium phosphate (per mg): J1100
- Celestone (per 3 mg): J0702
- Celestone (per 4 mg): J0704
- Depo-Medrol (40mg): J1030
- Depo-Medrol (80mg): J1040
- Kenalog/Triamcinolone (per 10 mg): J3301
- Toradol/Ketorolac (per 15mg): J1885 (don’t forget the 96372 code if injected intramuscular)
- Methocarbamol – Robaxin (up to 10 ml): J2800 (don’t forget the 96372 code if injected intramuscular)
- Synvisc 3 dose (per 2 ml syringe): J7325
- Synvisc One (per 6 ml syringe): J7325S
- Versed (per mg): J2250
- Fentanyl (0.1 mg): J3010
- Diphenhydramine – Benadryl (injection up to 50-mg): J1200
- Botulinum toxin type A – Botox, Dysport (per unit): J0585
- Botulinum toxin type B – Myobloc (per 100 units): J0587
Electromyography (EMG) & Nerve Conduction Studies (NCS)
- Sensory NCS (each nerve): 95904
- Motor NCS w/o F-wave (each): 95900
- Motor NCS with F-wave (each): 95903
- H-reflex (gastrocnemius/soleus): 95934
- H-reflex (other than gastroc/soleus): 95936
- Blink reflex (orbicularis oculi): 95933 (only once per study)
- EMG guidance during botulinum toxin injections: 95874
- Add modifier -26 if you don’t own the EMG machine you’re using
- EMG w/NCS, each extremity, “limited” (4 or fewer muscles): 95885
- EMG w/NCS, each extremity, “complete” (5+ muscles, innervated by 3+ nerves or 4+ spinal levels): 95886
- EMG w/o NCS on same day: one extremity = 95860, two extremities = 95861, three = 95863, four = 95864
- Cranial nerves
- EMG (unilateral): 95867
- EMG (bilateral ): 95868
- Note: EMG needles can not be billed separately, as they are included in the EMG codes
- Muscle testing before the study
- Extremity w/o hand (must include a report of this): 95831
- Hand: 95832
- 2013 CPT Coding Changes for Nerve Conduction Studies – Effective January 1, 2013
- Each conduction study is counted as one for sensory, motor with or without F-wave, or H-reflex. Orthodromic and antidromic tests on the same nerve count only once.
- Example: Bilateral sensory and motor median and ulnar NCS is performed. This is eight (8) separate tests, so the proper code now is 95910. Adding a radial sensory on one side would then make it a 95911.
- 1-2 NCS = 95907
- 3-4 NCS = 95908
- 5-6 NCS = 95909
- 7-8 NCS = 95910
- 9-10 NCS = 95911
- 11-12 NCS = 95912
- 13+ NCS = 95913
Evaluation and Management (E&M) codes
- New patients
- Straightforward – 10 minutes: 99201
- Straightforward – 20 minutes: 99202
- Low complexity – 30 minutes: 99203
- Moderate complexity – 45 minutes: 99204
- High complexity – 60 minutes: 99205
- Established patients
- Brief – 5 minutes: 99211
- Straightforward – 10 minutes: 99212
- Low complexity – 15 minutes: 99213
- Moderate complexity – 25 minutes: 99214
- High complexity – 40 minutes: 99215
- Independent medical examination (IME): 99456





This is one of the best lists for these type of procedures I have been able to find. We are new to coding the Epidural Steroid Injections and we are trying to make sure we are charging all of the correct codes. Still a little iffy on the Fluoro-also, when to charge supply codes and when not to charge them separately.
I would love it if this was updated with the new 2015 codes
I disagree with you on the example given for NCV code.
Example: Bilateral sensory and motor median and ulnar NCS is performed. This is four separate tests, so the proper code now is 95908.
Since the studies were performed bilaterally, the correct should be 95910. Because bilateral testing is often necessary and therefore the nerves are counted separately. Since four tests are performed individually on each extremity, they should be added together to get the right code.
You are absolutely correct. Thanks for pointing out my miscalculation. It is indeed 8 nerves, so 95910 is correct. I have made the correction above.
Good afternoon,
I have a pain doc that performed a common peroneal nerve block and need to know which would be the best code to bill. My research has brought me to 64450 but it does not look correct to me. Any help would be great!
Thanks,
That is the one I would use as well.
Hi, recently my billing manager stopped billing 77002, 77003, 76000, 96360 for an epidural procedure. She said everything is all ‘bundled’ now as of new change in 2013 CPT coding. Is that true? I’m taking a hit in my RVU production. I need to clarify this.
Also what code may I use for moderate sedation?
You can still use 77003 for interlaminar ESI, but not for transforaminal ESI. 77002 can still be billed for non-spinal fluoro use, such as for hips, knees, shoulders, trochanteric bursa, etc.
I have never used 76000 or 96360.
Moderate sedation CPT codes are listed above in the post, but I have never used them b/c I use local instead.
Paul we have a mutual friend I believe, Azlan? Anyway, I am starting my pain practice and was trying to develop my own superbill. This is invaluable!! Thank you sooooo much!
Chris, I just got off the phone with my friend Paul. Please forgive the mistake….omg!
Need the CPT code for a saphenous nerve block. Some say use the 64447 as it is a branch of the femoral nerve other say use the 64450.
Your opinion?
Thank you
What is the proper way of billing the levels? example
Medial Branch block left c5, c6, c7, c8
previously I would add all the levels in the computer and now the new biller wants the number of levels instead.
thank you
That’s a simple 4-level MBB.
64490
64491
64492 x 2 units
Thank you. I’d figured that, but they want me to list all the cpt codes like this.
64490 left c5
64491 left c6
64492 left c7
64492 left c8
Can I even do it like this??
This is how they want it listed in the system.
Sonia
Sonia, I’m not sure how they are listed in a particular system, but from a physician procedure coding stand point, those are correct. Keep in mind that 64490 can be billed for any cervical facet injection or medial branch block level; so listing it as “64490 left c5” seems silly. Good luck.
I just wanted to point out about the codes referenced above…64492 cannot be billed more than once per day, per notation immediately beneath the code in the CPT book. This is also true for 64495 for the L/S levels. From my understanding, the RVU’s for these 2 codes were calculated to be slightly more than 64491/64494 to allow for the fact that they might cover more than 1 level, but in the cases studied before these coding changes were made, most MBB’s were performed at only 3 levels.
Meagan, I have a “note” under the facet injection/block codes that I think explains what you say above. Let me know if it is not already clearly stated and I’ll think about changing the wording.
I work in a pain management office. for a medial branch block via RFA @ S1,S2,S3 I use codes 64635 and 64636×2. I was told to use 64640 instead?? Is this correct??
Also when coding injections for an in-office procedure dont forget to code for the drug and contrast.
I have never performed sacral (SI joint) radiofrequency ablation of the lateral branch nerves. I do know that you can not use the 64635 and 64636 codes though. I’m not sure if 64640 is correct, but I do know many insurance companies will consider RFA of the SI joint experimental. Good luck. If you figure it out, please come back and update us.
And yes, always remember the Q- & J-codes for contrast/steroids (I have those listed above under all the injections, and before the EMG/NCS)
What about manual therapy codes following transdermal compound use.
Mobilizations, soft tissue manual releases, accupuncture.
Absolutely no clue about this.
Hi, I was wondering what the correct ICD 9 code would be for a sacrococcygeal joint radiofrequency would be. Any help would be appreciated.
Thanks!
I know some that are performing RFA at the L5 dorsal primary ramus, and then the lateral branches of S1, S2, S3.
L5 is being billed as 64635
S1, S2, and S3 are billed as 64640 (for each one).
I haven’t done this yet, so I don’t know about denials, but the physician that told me said she hasn’t had any problems with it.
Hey Everyone!
So I am having this issue with a new(er) Neuropathy treatment using the 64450. I bill as follows:
64450 LT 1 unit
64450 59-51 4 units
64450 RT 1 Unit
64450 59-51 4 units
Medicare is not paying a whole lot and when I spoke to them on the phone they recommended:
64450 50 1 unit
64450 50-59 4 units
Still trying to figure out how to get the maximum amount I can get when I was billing originally for 10 units (5 each side) HELP!!!
I think the Medicare representative provided the incorrect unit count.
64450 50 12 unit
64450 59-50 8 units
When coding Lumbar Radio frequency 64635,64636 on the add on coded 64636 do you use a modifier. I been getting Medicare denials for wrong modifier
We never use a modifier for lumbar RF. What modifier are you trying to use?
I have been getting the same denial for the radiofrequency Medicare is denying
64635
64636
64636- STATES DUPLICATE
should I try billing
64635
64363-x2 OR
64635
64636
64636-59
What is your opinion???
I am having the same problem with Medicare! I don’t see anybody responded to your question, have you found a way to resolve the issue? I could really use the help!
Help!!!!
I’m new at pain management and I am trying to bill 3 level lumbar neuroplasty and I can’t the find the billing codes Can anyone help me. Thank you very much
Unfortunately, I’m not sure what you mean by “neuroplasty”. Do you mean “Epidural Adhesiolysis”? 62264 and 62263 are the codes for epidural adhesiolysis, but I don’t perform these so I really can’t help other than that. Good luck.
What is the correct cpt code for ganglion impar nerve block for coccydynia? Much confusion about correct coding.
Thanks
Hopefully this page helps you: https://thepainsource.com/ganglion-impar-block-under-fluoroscopy/
Dr did a fluor guided contrast bilateral c2-3 and c3-4 facet injections and 3rd occipital nerve block. i have 64490(50),64491(50). how would I code for occipital nerve block?
We use the code 64450 (other peripheral nerve) for third occipital nerve (TON) blocks. More importantly than the actual joint, for medial branch blocks, you need to look at the actual medial branch nerves (facet nerves) that were blocks. For instance, did the physician block the TON, C3 and C4 nerves bilaterally; that’s what I’m getting from the question. In that case, you’re absolutely right about the 64490-50 and 64491-50. Sometimes insurances will deny the 64450 code, but I would give it a shot as it is anatomically needed in ordered to block the entire C2/3 facet joint.
I just took over the billing and have a ton of rejects regarding the G0434 code for Medicare, any suggestions?
Sorry Olivia. Unfortunately I can’t help you there; we don’t do any in-office drug screens. We send everything out to be run.
You can only bill 1 unit of the G0434. How many are you billing for and what DX are you using?
To bill medicare on the G0434 you have to have a QW modifier. You need to add to your claim the billing provider, supervising provider, ordering provider, referring provider and of course your facility name and CLIA waiver number. I had so much trouble getting medicare to pay on this code. Once you add all this information
Can you please help me with the correct code for ganglion Impar Block
under fluoro. Thanks in advance.
Hopefully this page helps: https://thepainsource.com/ganglion-impar-block-under-fluoroscopy/
how to bill code 64640 for S1, S2, S3 rfa?
I believe we use the 64640 x 3 units for the S1, S2, S3 lateral branch RFA. Also use the spinal fluoro code of 77003.
What is the correct cpt code and icd 9 code for piriformis injection and piriformis syndrome?
I just use the trigger point muscle injection code of 20552, but add the fluoro or ultrasound codes if done with that guidance (as they definitely should be).
Hello. My name is Italo and I´m from Guatemala, Central America.
We do not usually use CPT coding in Guatemala, but I am opening a Pain Management clinic and would like to use CPT coding in order to calculate an objective pricing on our services. Does anyone know where can I find a CPT coding guide for Pain Management that includes value units??
Thank you so much for your help!!
Kind regards.
Italo, this link has info that came from the data from the American Society of Interventional Pain Physicians (ASIPP). Hope it is what you’re looking for.
https://thepainsource.com/total-rvu-work-rvu-pain-management-pmr-clinics-2014/
What is the correct code for Right lumbar sympathetic plexus block. Please suggest
I’d use 64520
Can we code 64450,64490,64491,64492,& 64483 for same Date of service. Please suggest.
Sounds like you’re talking about medial branch blocks for the C-spine. C2/3, C3/4, C4/5, C5/6.
I’d leave out the 64450. You’re probably trying that for the third occipital nerve which innervates the C2/3 facet joint. So along with the C3 medial branch nerve, it constitutes the 64490 charge.
Is fluoroscopy included in nerve block injections? Or shoul I be using 77002? What about with stellate ganglion blokcs 64510 does it include fluoro? If it doesn’t would the fluoro code be 77002 or 77003?
I’d use 77002
This is one of the best lists out there, and was wondering if this is going to be updated with the 2015 revised codes. Please and thank you !!
I’m a certified coder of 20+ yrs but new to pain mgmt.
I’ve been trying to look for some good coding courses that would help me with this challenging field.
Any suggestions would be greatly appreciated!!
Thank you.
This article is one of the best things I’ve come across. Thank you so much. 🙂
At the top of your web page it says, “These have all been updated for the most recent 2013 changes.” Well, it’s the end of 2014 & almost 2015, my question here is, How often does this get updated & where do you get your sources from? Just wondering, kind of like to know. I noticed nobody has ever or that I have seen asked that question. If you don’t mind letting us know please.
What CPT code would you use for “anesthetic and steroid inj left posterior superior iliac spine?
That would have to be a trigger point injection, so 20552
I’m getting denials from Medicare for code 64520, how should I be billing this? I’ve tried billing with -50 or with 2 units and its still getting denied. Please help.
I am getting denials from Medicare for this procedure as well and cannot figure out why. Modifier 50 is not applicable because the physician did just a unilateral procedure. I am going to file with a 59 modifier to see what happens.
We will be doing medial branch blocks 64493 at the office with the C-arm and wanted to know how to bill the facility fees and the professional fees and the tray of instruments. We have never done this at the office before it’s going to be our first time and I do not know how to properly bill it. Thank you in advance for all of your help.
Sonata, there won’t be any facility fees when done in the clinic setting. Facility fees are for ASC or hospital procedures only. Instead, there is a single global fee that includes the instrument/supplies. The C-arm codes are also bundled with the facet medial branch blocks too. I have an article on my site that explains the coding/billing for MBBs and RFAs.
We are getting payor path rejections beginning in 2015 when my pain management physician does a MBB followed by an RFA on one side, then goes back on a later date and does MBB followed by RFA on the contralateral side. The initial side is being paid with no problems; when I file for the contralateral side, I am getting rejections stating that the patient is in a global period for that service or test???? So if I file my initial MBB coding with RT or LT modifiers as appropriate, then the follow-up RFA with that RT/LT modifier, when I bill for contralateral side and use the other side modifiers, do we think that might solve this issue?? I am so confused! Again, this just started in 2015.
Debi, we always use those Lt and Rt modifiers for that exact reason. We haven’t had any “global period” issues that I’m aware of.
Hello: Need help in cpt code 27096, performed bilateral, UMWA paid in 2012, now they are asking for refund, unless I show the proof that 27096, 50 is approved by Medicare. How do I show the proof? I cold not find any CMS policy to prove this. Thank you
Sacroiliac denervation. Right L4 medial branches L5 DPR & Right S1, S2, S3 lateral branches Radiofrequency lesioning. Only L5-1 and S1-4 were done as patient could not tolerate the procedure. How would you bill this to include all modifiers? Thank You.
How would you code for Medial Nerve Branch Radiofrequency procedure using a Halyard (formerly Kimberly-Clark) Cooled Radiofrequency Pain Management RF generator?
64635 or unlisted?
As long as the machine gets the temperature at or above 60 degrees Celsius, you’re okay billing the regular thermal RF codes.
Hi, I am working in a group for Anesthesiology – Pain Medicine, I observed that Medicare is not paying 77003 and 77002 separately, these services they always bundled with other services. My question is that is there any way to get payment for these services separately?
Your prompt response will be appreciated.
Can my physician bill for an epidural steroid injection as well as a lumbar facet injection at the same setting?
I don’t know that I’ve ever done both on the same visit, but sure. One of those procedures will likely be reduced payment though.
When Billing out a 64517 Humana is asking for an Anesthesia Code. Should this be billed along with 64505?
Hello! I am having problems with some carriers refusing to pay for the U/S guidance for the piriformis injection. We use 20552 for injection and 76942 for u/s guidance. Even when appealed with office notes I am getting rejections. Any suggestions?
Can you please help with what is the correct cpt code to bill chronic pain programs?
HI Dr,
Could you please help me why my billing INJ. code got denied as Quantative,Unit,Measure required even I had information at location box 19 (1500 CMS form). Please advice what I need to do to get pay on drug injection code
J1030,j3490,j3420,j1020,j1885,j1040 etc…Thank You
I am wondering what are the payable DX for CPT J0702 for Medicare billing?
Hi Debbie,
Payable Dx code for J0702 is 722.52.
what code would I use for a rfa @ T12-L1? cervical or lumbar?
Good question. I’d use 64635 for a lumbar RF.
IS THERE A CPT CODE THAT I CAN ADD FOR MY DOCTOR WHO TREATS PAIN, WHEN HE GIVES OUT TWO OR THREE SCRIPTS.FOR EXAMPLE IF THE WRITES NORCOR AND THEN WRITES XANAX IS THERE A CPT CODE TO CHARGE FOR TWO SCRIPTS?
You can’t charge for the number of scripts given. You can only bill for time taken or complexity of case. If he/she wrote 10 scripts, it doesn’t matter.
I work for a large Orthopedic Group and one of the Dr’s I bill for provides Genicular Blocks to the knee. He uses CPT 64445, 64447, 64450 & 77002 when he does these procedures. Are you familiar with this “newer type” of procedure and if so do you have any insight to help me maximize his reimbursements? I’ve checked CMS website but they do not yet recognize “Genicular” nerves. Thank you in advance.
Everyone I know uses either 64447 (femoral nerve block) or 64450 (other peripheral nerve). The RFA of these genicular nerve branches would be 64640 for the first one, and 64640-59 for the second one.
I haven’t started doing these yet, so I can’t comment with personal experience.
Dr. Faubal, why use the 59 modifier for genicular RFA?
Could you please help me with billing a INJ. I’m not sure what Cpt codes we can use or if their is one.
RFD, T5 to T8 .
Not sure what RFD is
Any suggestion for CPT for RFTC on a sacral neuroma
I am just wondering what code is used for injection of steroid/anesthetic in the joint between L5 transverse process and ilium or sacrum.
Thanks.
.. in Bertolloti’s syndrome, I mean
That would be the L5/S1 facet joint, so 64493 is appropriate.
Impar block ganglion ulnar nerve. Is there an billable code for workers’ comp?
I’m not sure what you’re trying to say here. An impar ganglion block doesn’t have anything to do with the ulnar nerve.
HI. I am performing lumbar medial branch blocks from L2-S1, 5 levels and billing for 4 levels. My billing department is telling me that I can only bill for 3. In the past I was adding 2 units to the 64495. In the 2015 CPT code book it states that 64495 can only be used once per day. Can you explain this please?
medial branch block lumbar or sacral (1st level): 64493
medial branch block (MBB) – lumbar or sacral (2nd level): 64494
medial branch block (MBB) – lumbar or sacral (3rd level): 64495
1. When billing SCS trial with two leads, do you suggest 63650 for the first lead and 63650-59 for the second lead or do you use modifier 50 for bilateral?
2. When billing piriformis and hip bursa injections performed under fluoro on the same day
a. 20610 and 20552-59 and 77002
b. 20552 and 20610-59 and 77002
c. something else?
Dr. Faubel,
In your experience, is it appropriate for the physician or the facility to charge for moderate sedation services provided during interventional pain procedures? We are in a battle of the wills with our pain physician over this issue. He feels it is appropriate to use the 99144 code (which we understand that Medicare will not reimburse), while the facility would code using 99149. We do not want to double-bill the patient/payor. I’ve sounded other pain practices in my region, but all use anesthesia services rather than nurse-provided sedation. Thanks in advance.
Sorry, I don’t have a good answer for you. I don’t use conscious sedation except for spinal cord stimulator trials and kyphoplasties, and for these, an anesthesia group comes in to provide the sedation and bill separately.
The vertebroplasty and kyphoplasty codes need updating:
http://news.aapc.com/solidify-your-vertebroplasty-and-kyphoplasty-coding/
Thanks for the heads up, Fred. I just updated them.
My CRPS/pain management neurology office started to no longer perform bilateral nerve blocks on the same day. I assume this is so they can bill separately and receive more money from Medicare. This practice seems unethical for multiple reasons, including requiring a patient to undergo sedation twice instead of once, which creates additional risk, as well as prolonging patients ‘ pain because they have to wait a week or more as these procedures are only done 1 day a week and appointments are limited, often increasing wait times therefore prolonging patient pain and suffering. Thank you for your time and knowledge in responding to a patient rather than a
billing staff. I appreciate your timely answer as I receive regular, multiple sites blocks so this affects me imminently and greatly.
I’m not sure what “nerve blocks” you’re referring to. Which nerves?
what cpt code is used to bill for Lumbar hardware block?
Never heard of this
My physician performed a Lg joint injection (20610/J0702), on this same day the patient was also seen for an EMG study (95912/95886) here in the office. We have billed the injection w/ a -59 and it was paid but the insurance has denied the EMG as “included in the Lg joint injection” and said cannot be billed/paid separately. What, if anything can I do to get this “unbundled” from the injection? Thank you in advance for your help!
For the Genicular nerve block: 64450, would the units be the number of places the physician injects? or is it always X3 units? We are doing our first one and I wanted to make sure that we are billing it appropriately.
The units are billed per separate nerve injected. The standard is to block 3 separate nerves. The superior medial genicular nerve, superior lateral genicular nerve, and inferior medial genicular nerve. It’s NOT different parts of a single nerve, these are three separate nerves.
When billing from an in-office based setting, can the supplies for the procedures, such as the needles and drugs for the conscious sedation be billed or are they bundled into the procedure codes?
Conscious sedation has a separate code that I believe includes the drugs used. Definitely can’t bill for the needles.
Billing Trigger points and g.trochanter injection together? Will I be able to bill these procedures together? I also used fluro for needle guidance secondary to body habitus for the g.trochanter injection…
I had talked to someone who felt I should do them on separate days… seems silly to me but reimbursement may not feel the same way…
Hey Jon. I’m unsure about this. I believe I’ve billed them together, such as a piriformis muscle and GTB on the same visit; don’t think it gets denied.
The medial branch joint stops at L5. S1-S4 are not part of the medial branch. To block these nerves code 64450(other peripheral nerve) is used. Same with RFA’s, except the S1-S4 is coded per nerve with 64640 with mod 59.
Can we bill 77002 with 64450 g-block?
I do, and I don’t believe we get any denials for it.
Not sure if this blog is still active. I am trying to get reimbursed for disposable supply items used during esi and blocks. How is everyone doing it these days.
No insurance company in my area reimburses for disposable supplies such as gloves or needles or syringes. Sorry.
I am billing for 3 ml of omnipaque Q9966 how many units do I bill?
3
on CPT code 20553, it is for 3 or more muscles, can this be billed as bilateral if it is for 3 muscles on left and 3 muscles on the right? Or do i just bill the 1 unit as the description says “3 or more muscles”
I believe it is 3 or more muscles no matter the side it is done on.
Since the description of 64421 is Intercostal nerves, multiple, regional block, can you multiple units be billed?
Nope. You only get to bill this once. Multiple is multiple, no matter if it is 3 levels or 6
Hi,
Radiofrequency denervation of cervical medial branches under fluoroscopic guidance – your website suggests 64633-64634.
However, the CPT book state that for radiofrequency, it is 64999.
64999 is definitely not the correct code for RF of a cervical medial branch nerve.
Here’s s0me updated information for your site.
This is from CPT Nov. 2015
Surgery: Nervous System
Question: When a physician injects the superior medial and lateral branches and inferior medial branches of the left genicular nerve, is code 64450 reported three times or just once for the left genicular nerve?
Answer:It is appropriate to report code 64450, Injection, anesthetic agent; other peripheral nerve or branch, for the genicular nerve block of three branches of this nerve around the knee joint; however, code 64450 is reported just once during a session when performing the injection(s). Although one, two, or more injections may be required during the session, the code is reported only once, irrespective of the number of injections needed to block this nerve and its branches.
This is from CPT June 2012
Surgery: Nervous System
Question:May code 64640 be reported for each individual peripheral neurolytic nerve destruction procedure performed at the L5, S1, S2, and S3 nerves?
Answer: Yes. When performing individually separate nerve destruction, each peripheral nerve root neurolytic block is reported as destruction of a peripheral nerve, using code 64640, Destruction by neurolytic agent; other peripheral nerve or branch. In this instance, for peripheral nerve root neurolytic blocks (destruction) of L5, S1, S2, and S3, code 64640 should be reported four times. The coder should append modifier 59, Distinct Procedural Service, to the second and subsequent listings of code 64640 to separately identify these procedures.
Great information. I would argue that the first question/answer regarding the genicular nerve blocks is incorrectly worded. The physician isn’t injecting/blocking three branches of the genicular nerve, they are blocking three separate and distinct nerves. The superior lateral genicular nerve, the superior medial genicular nerve, and the inferior medial genicular nerve.
The above is information is from CPT Assistant June 2012 and November 2015.
what is the CPT code for pulsed radiofrequency of the peroneal nerve??
Is there an RF procedure of the sacrococcygeal joint. Performed a ganglion impar injection and interarticular SC injection with good relief. Pt with hx of RF procedure to the sacrococcygeal joint. Can’t find any information about this procedure or how it would be billed. Any information would be appreciated
Absolutely. Surprised I haven’t made a post about that yet. I’ll get on that.
What CPT would be used for anterior neck block.
WHEN WILL THE 2017 CODES BE UPDATED?
As of January 1st, 2017, the CPT codes have changed for ESIs
New Codes:
62320 – Injection(s), of diagnostic or therapeutic substance(s) (e.g., anesthetic, antispasmodic, opioid, steroid, other solution), not including neurolytic substances, including needle or catheter placement, interlaminar epidural or subarachnoid, cervical or thoracic, WITHOUT IMAGING GUIDANCE (previous code – 62310)
62321 – WITH IMAGING GUIDANCE (i.e., fluoroscopy or CT)
62322 – Injection(s), of diagnostic or therapeutic substance(s) (eg, anesthetic, antispasmodic, opioid, steroid, other solution), not including neurolytic substances, including needle or catheter placement, interlaminar epidural or subarachnoid, lumbar or sacral (caudal), WITHOUT IMAGING GUIDANCE (previous code 62311)
62323 – WITH IMAGING GUIDANCE (i.e., fluoroscopy or CT)
62324 – Injection, including indwelling catheter placement, continuous infusion or intermittent bolus, of diagnostic or therapeutic substance(s) (e.g., anesthetic, antispasmodic, opioid, steroid, other solution), not including neurolytic substances, interlaminar epidural or subarachnoid, cervical or thoracic, WITHOUT IMAGING GUIDANCE (previous code 62318)
62325 – WITH IMAGING GUIDANCE (i.e., fluoroscopy or CT)
62326 – Injection, including indwelling catheter placement, continuous infusion or intermittent bolus, of diagnostic or therapeutic substance(s) (eg, anesthetic, antispasmodic, opioid, steroid, other solution), not including neurolytic substances, interlaminar epidural or subarachnoid, lumbar or sacral (caudal), WITHOUT IMAGING GUIDANCE (previous code 62319)
62327 – WITH IMAGING GUIDANCE (i.e., fluoroscopy or CT)
Deleted Codes:
62310 – Injection, single, of diagnostic or therapeutic substance(s) (including anesthetic, antispasmodic, opioid, steroid, other solution) not including neurolytic substances, including needle or catheter placement, includes contrast for localization when performed, epidural or subarachnoid; cervical or thoracic
62311 – lumbar, sacral (caudal)
62318 – Injection, including indwelling catheter placement, continuous infusion or intermittent bolus, of diagnostic or therapeutic substance(s) (including anesthetic, antispasmodic, opioid, steroid, other solution), not including neurolytic substances, includes contrast for localization when performed, epidural or subarachnoid, cervical or thoracic
62319 – lumbar, sacral (caudal)
Is there a CPT code to bill for reviewing Opioid risk screening tools/questionnaires like the COMM or the SOAPR-R, ORT, etc.?
I have a rep that is selling a screening questionnaire stating they can get our practice 40 extra dollars per questionnaire. We are actually in the process of implementing this practice wide but we didn’t think we were going to get paid for it. Is this possible? If so, do you happen to know what the codes are and the process of billing to review the questionnaire?
I don’t know that code. Never heard of one. I’d guess the insurance companies would consider that bundled with the E&M code. Please share if you find out.
How do you code for migraine/cluster headache?
Do you use 64400 and 64505 with 50 modifier?
How do you appeal for denial?
Will the Pain Source be updating the cpt codes for 2017?
We have a pain clinic physician who is wanting to report the new CPT 64486 TAPS by single injection for chronic pain management of the transverse abdominus. Since 64486 seems to be indicated for post op pain management I believe that CPT 64450 injection other peripheral nerve would be a better choice.
Sorry, but I’m not familiar with this procedure.
Thanks for the above information, it is fantastic! I am a physiatry resident and future pain management doc and find this extremely helpful.
Can I suggest adding a two more categories of codes?
First, Office Modalities:
Acupuncture
-with electrical stimulation: 97813
-without electric stimulation: 97810
Diathermy (Microwave): 97024
Heating pads / cold packs: 97010
Self-care / home management training: 97535
Theurapeutic ultrasound: 97035
Traction: 97012
Transcutaneous Electrical Nerve Stimulation (TENS): G0283
Second, for us D.O.’s, we do OMT = Osteopathic Manipulative Treatment:
OMT 1-2 body regions: 98925
OMT 3-4 body regions: 98926
OMT 5-6 body regions: 98927
OMT 7-8 body regions: 98928
OMT 9-10 body regions: 98929
(note: use 98928 or less if OMT done in conjunction with an injection and 98927 or less of OMT done in conjunction with epidural)
EXCELLENT suggestions. Thank you. I’ve added them above.
Hi,
My provider does Trigger point injections and uses the following verbiage…
“then gave the patient trigger point injections in cervical paraspinous and trapezius region. I used dry needling technique with 25-gauge, 1.5-inch needle, and 1 mL of injectate was given at each level. Total injectate was 40 mg of preservative-free Kenalog, 4.5 mL of 0.25% Marcaine, and 4.5 mL of 2% lidocaine. Band-Aids were placed over all injectate sites. Patient was hemodynamically and neurologically intact upon discharge. Follow up in two months”
When she refers to the dry needling technique does this change it from a 20552-20553 to an unlisted code?
Thank you for your help!
Hi,
Has anyone had a chance to review my comment yet??? Thank you!
Nope. It would still be 20552 or 20553. The dry needling is just part of the procedure but shouldn’t change the billing/coding.
I have been diagnosed with occipital neuraglia ICD9 (723.8) & ICD10 (M53.82)
I have received the nerve block injection: CPTcode 64405,77002,J1040,J34901PF1
These injection give immediate relief therefore this is the correct diagnosis (after years of being treated for migraines)
The insurance companies deem these CPT codes “medically unnecessary” so they do not pay for the injection…Any advice on how to get nerve blocks for the lesser and greater occipital nerve covered….thanks
Unfortunately not. Try to change insurance companies if you can. Ask the doctor if he/she is aware of a policy that covers these injections.
Hello, are there any new updates to codes since this is showing; “As of 2015?”
As of 01/01/2017, the ESI CPT codes have been updated as follows:
62320 – Interlaminar epidural or subarachnoid, cervical or thoracic, without imaging guidance
62321 – with imaging guidance (i.e. fluoroscopy or CT)
62322 – Interlaminar epidural or subarachnoid, lumbar or sacral (caudal), without imaging guidance
62323 – with imaging guidance (i.e. fluoroscopy or CT)
If indwelling catheter placement is included in procedure, CPT codes are 62324-62327 for cervical and lumbar, with and without imaging guidance.
*N0te: Do not report 62320-62327 with 77003, 77012, or 76942
Cervical Epidurals have a new code as of 2017- 62321 with fluro
Lumbar interlaminar/caudal – 62323 with fluro
Your website should be updated
Hi I’m new to pain management. I’m confused, are facet injections the same thing as medial branch blocks? I thought lumbar MBB codes were 64493, 64494, 64495, but I’m also seeing them listed as facet injection codes. My doc wants his pt pain free before she gets off the table. His plan is as follows: right L4/5 facet; then a right L4/5 mbb if that doesn’t work; and if neither of those work, then a LESI L4/5. I know the LESI code is 62323. Thanks for your help!
The codes for medial branch blocks and facet steroid injections is the same. The difference is that you need to block two medial branch nerves in order to kill the pain from one facet joint. So for the right L4/5 facet joint, he/she would have to block the L3 and L4 medial branch nerves on the right side. But regardless, this is billed as ONE facet joint, so just the 64493. You really can’t bill for two facet joints if the doctor does a medial branch block AND intraarticular facet joint steroid injection. It’s still just the 64493.
I am looking for the correct CPT code for right suprascapular RFA. Can you help me?
I’m not sure anyone would do a suprascapular nerve thermal RFA. Pulsed RFA is common for this nerve, but a thermal ablation would kill off the nerve supply to the supraspinatus and infraspinatus muscles causing wasting away. Pulsed RF is for pain management of should pain, but isn’t reimbursed by insurances. BUT, if the doctor is doing a true thermal suprascapular nerve RFA, the correct code would likely be 64640 (other peripheral nerve ablation).
The CPT Codes for the interlaminar epidural steroid injection has changed in 2017. I think you should update it.
CPT Code for interlaminar- cervical or thoracic: 62321
CPT code for interlaminar- lumbar or sacral: 62323
What is the correct CPT code for Bilateral third occipital nerve radioofrequency ablation under fluro?
Most people do the third occipital nerve RF in addition to the C3 facet joint medial branch RF and therefore bill for denervation of one cervical facet joint. 64633 would be the correct code. Otherwise, if you just do the TON, you could bill for a peripheral nerve RF 64640.
What code are you using to bill Splanchnic Nerve block for abdominal/viseral pain?
Your 2015 coding sheet has been such a great resource for my staff…. would love to see a new updated PDF version with the 2017 coding changes.
Different coding opinions from pro coders/hospital coders: Anterior scalene anesthetic injections . .most are for neurogenic thoracic outlet syndrome: . . .patient was placed in a supine position on the CAT scan table. After placement of an overlying skin marking device, limited axial images were obtained to select a trajectory into the anterior scalene muscle. Local anesthesia was achieved with bupivacaine. A 25-gauge needle was then placed into the skin and repeat imaging was obtained. There was significant patient movement between initial imaging and marking and a second location was marked and anesthetized. A 25-gauge needle was advanced with intermittent serial axial imaging into the anterior scalene muscle. Position was verified. 0.1 mL of diluted Omnipaque 180 (1:20 with normal saline) was injected via micro-tubing connected to the needle. Repeat imaging demonstrated good position of the contrast material. The intramuscular anesthetic was then slowly injected via micro-tubing connected to the needle. Repeat imaging demonstrated continued spread with good distribution of the contrast material.
Intramuscular Anesthetic: 2 mL of 0.5% bupivacaine
IMPRESSION. Left Anterior Scalene Anesthetic Injection
Is this 64415 or 20552 –
This list is amazing! Thank you!!
I have some serious confusion surrounding genicular nerve blocks, genicular RFA, and the use of flouroscopic guidance for the medial superior genicular nerve, lateral superior genicular nerve, and the medial inferior genicular nerve. We used to bill these codes with 3 units and then with CPT 77002 for flouroscopic guidance. Now, Medicare isn’t paying for the flouro when billed with 64450 or 64640. They used to pay it with a 59 modifier. My questions lies in what everyone else is seeing…..According to NCCI Edits that were published this year you can now only bill 1UOS for 64450:
8. CPT codes 64400-64530 describe injection of anesthetic agent for diagnostic or therapeutic purposes, the codes being distinguished from one another by the named nerve and whether a single or continuous infusion by catheter is utilized. All injections into the nerve including branches described (named) by the code descriptor at a single patient encounter constitute a single unit of service(UOS). For example:
(1) If a physician injects an anesthetic agent into multiple areas around the sciatic nerve at a single patient encounter, only one UOS of CPT code 64445 (injection, anesthetic agent; sciatic nerve, single) may be reported.
(2) If a physician injects the superior medial and lateral branches and inferior medial branches of the left genicular nerve, only one UOS of CPT code 64450 (Injection, anesthetic agent; other peripheral nerve or branch) may be reported regardless of the number of injections needed to block this nerve and its branches.
I am having difficulty in getting an actuate CPT code for a sacrococcygeal joint injection. My provider coded 20605, but the Dx code M53.3 will not support that code and he doesn’t agree with coding 62323, yes, the coccyx is a joint, however , in coding, I believe it is part of the spine, what is your recommendation?
I always do a ganglion impar block (64520) along with the sacrococcygeal joint injection. Code it with M53.3. Definitely not a 62323 because it is in no way an ESI.
The codes needs to be updated as there are many which has been changed or updated. The coding pattern has been changed for some codes
Over all , Amazing web for Pain procedures coding