By Chris Faubel, MD —
Although once thought to have no innervation and therefore unable to produce pain, the intervertebral disc has been found to be quite well innervated. It is still believed by some that only the outer 1/3 of the disc has innervation, though others have found nerve endings much deeper (especially in diseased/damaged discs).
Nikolai Bogduk describes two large plexuses that supply the intervertebral discs (IVDs) and other structures (anterior and posterior longitudinal ligaments, and vertebral body).
- Anterior plexus
- Posterior plexus
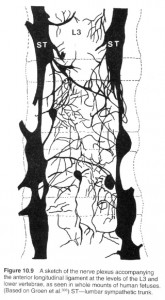
The anterior plexus covers the anterior longitudinal ligament (ALL) and is formed from branches of the sympathetic trunks on either side of the vertebrae. These sympathetic trunks run along the anterolateral length of the spine. Branches from the sympathetic trunk form a patchwork-type of plexus seemingly haphazardly spread along the anterior vertebral body and ALL. These same branches get more coordinated and form segmental grey and white rami communicans (only grey rami below L2). These grey rami from the sympathetic trunk send off little branches into the anterior and lateral outer 1/3 of healthy intervertebral discs (and even deeper in diseased discs). These fibers then proceed posteriorly to join the ventral ramus at that level, and then centrally through the dorsal roots to the spinal cord and up to the sensory cortex.
- Note: These nerve endings from the anterior and lateral disc may also travel anteriorly with the grey ramus to the sympathetic trunks and go up and down a few levels before entering the spinal cord.
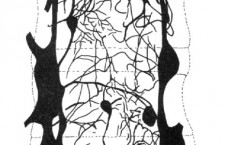
The posterior plexus is formed primarily from the sinuvertebral nerve and runs along the posterior aspect of the vertebral body and disc with the posterior longitudinal ligament (PLL).
- The sinuvertebral nerve is a branch off the ventral ramus after it exits the intervertebral foramina. This nerve loops back around and reenters the foramen, and then to the posterior spine anterior to the spinal cord. See the colored diagram below.
Note: The dorsal (pure sensory) and ventral (pure motor) roots from the spinal cord join together in the intervertebral foramina (IVF) to form a mixed spinal nerve [mixed because it contains both sensory and motor fibers] and then split into two mixed nerves: a dorsal ramus and a ventral ramus.
Clinical relevance: Pain medicine practitioners have used this information about the innervation of the IVD to devise techniques to both diagnose and treat discogenic pain.
- Discography – Diagnostic test used to diagnose discogenic pain from annular tears by pressurizing the IVD with contrast dye and therefore theoretically activating the pain fibers (looking for pain similar to what the patient has been experiencing). This isn’t performed much anymore because insurers don’t cover it.
- IDET (Intradiscal Electrothermal Therapy) – A needle is inserted into the pathologic disc on the opposite side of the annular tear. A heating wire is then advanced through the needle and toward the tear. This wire is then heated in an attempt to repair the tear and cauterize the painful nerve endings.
- Local anesthetic to the sinuvertebral nerve in order to diagnose the pathologic level. This is difficult and more dangerous to perform because you have to get to the anterior portion of the spinal canal. This technique wasn’t shown to be more effective than discography, which is controversial itself.

















nicely done!
Thanks 🙂