Posted by Azlan Tariq, D.O.
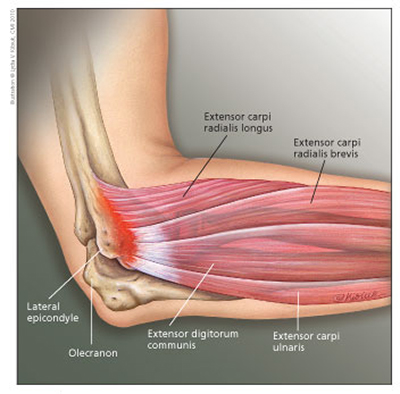
Also known as “tennis elbow“, lateral epicondylitis is a very common condition seen in overuse of the extensor tendons of the forearm. It can occur from many different activities and not just from playing tennis. Even though the condition has a high prevalence, there are not many high quality trials that support the numerous treatment options available.
Prevalence:
Typically affects patients 40 years or older with a history of repetitive activity during work or recreation. If untreated, it can persist of an average of 6 to 24 months 1 . No association has been found with gender.
Diagnosis:
Patients present with history of occupation or activity-related lateral elbow pain. Symptoms are reproduced with resisted supination or wrist dorsiflexion, and localized distal to the lateral epicondyle over the extensor tendon mass. Activities with gripping, wrist extension, and lifting are characteristically painful. Patients will exhibit a positive Cozen’s test. (Video). Significantly less or no pain when lifting objects with palm up, compared to palm down.
- ICD-9 code:
- 726.32 “lateral epicondylitis”
- ICD-10 codes:
- M77.11 “lateral epicondylitis, right elbow”
- M77.12 “lateral epicondylitis, left elbow”
Imaging:
Not required. Plain film radiography unable to demonstrate soft tissue changes but can reveal other causes of pain including loose bodies, fractures or osteoarthritis. Ultrasound and MRI can show changes of tendinosis, but these changes do not necessarily correlate with clinical symptoms.
Treatment:
Watchful waiting: One study showed that one year of watchful-waiting was comparable with physical therapy (PT) and superior to corticosteroid injections in alleviating complaints 2.
NSAIDS: Topical NSAIDs may provide short-term pain relief of a few weeks. Three studies found diclofenac and benzydamine to be effective 3. The evidence for oral NSAIDs is conflicting. Two studies have shown significant short-term benefit with diclofenac 150mg PO daily and one study showed no difference in pain between naproxen 500 mg daily and placebo.
Corticosteroid injection: Local injection has short-term benefit of two to six weeks in pain reduction, global improvement and grip strength, compared to other conservative management, per three studies 4. Benefit does not persist after six weeks. Oral NSAIDs and PT have greater benefit than injections at time periods greater than six weeks and in long-term follow-up greater than six months.
Learn about the lateral epicondyle steroid injection technique and tips HERE.
Extracorporeal shock wave therapy: A 2005 systematic review that included nine randomized controlled trials found strong evidence against using extracorporeal shock wave therapy
Orthoses: Despite the widespread use, multiple systematic research have shown no benefit of orthoses for lateral epicondylitis 5.
Laser therapy: Evidence shows no evidence of use of laser therapy for treatment of lateral epicondylitis.
Physical therapy: Exercise programs can reduce pain. Regimens should focus on eccentric instead of concentric phases.
Electrotherapy: Three studies have shown pain reduction with diclofenac and pirprofen iontophoresis after two to four weeks.
Ultrasonography: Data shows that it provides modest pain reduction over one to three months.
Mobilization and Massage: Insufficient evidence that deep transverse friction massage improves symptoms.
Acupuncture: Two systematic reviews, and one meta-analysis found that acupuncture leads to short-term (three days to two months) pain reduction.
Autologous blood injection: Clinical trials with comparison group receiving placebo lacking hence it is currently not recommended but does show promise.
Botox: Conflicting results. Shown to be less effective than corticosteroid injections.
Topical nitrates: A RCT of 86 patients compared a nitroglycerin transdermal patch with a placebo patch. The nitroglycerin patch reduced elbow pain with activity at two weeks, reduced epicondylar tenderness at six and 12 weeks, and increased wrist extensor mean peak force and total work at 24 weeks. At six months, 81 percent of treated patients were asymptomatic during activities of daily living. 6
Surgery: Recommended when conservative strategies fail to relieve symptoms after six to 12 months. Case series have favorable outcomes, but no randomized controlled trials have been performed.
Conclusion
1) Common condition seen with overuse of the extensor tendons of the forearm and presents with pain in lateral elbow. Positive Cozen test. Clinical diagnosis.
2) Always start with correcting errors of biomechanics. Initiate topical or oral steroids plus home exercise regimen. Can try watchful waiting depending on patients severity of symptoms and pain tolerance.
3) If symptoms do not resolve in 4-6 weeks, consider corticosteroid injection along with physical therapy with ultrasonography and/or NSAID iontophoresis.
4) If symptoms do not resolve after 4-6 weeks, consider topical nitrates or acupuncture.
5) If symptoms do no resolve in another 4-6 weeks consider surgery consultation.
REFERENCES:
1) Understanding prognosis to improve rehabilitation: the example of lateral elbow pain. – Hudak PL – Arch Phys Med Rehabil – 01-JUN-1996; 77(6): 586-93
2) Smidt N, van der Windt DA, Assendelft WJ, Deville WL, Korthals-de Bos IB, Bouter LM. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomised controlled trial. Lancet 2002;359:657–62
3) Green S, Buchbinder R, Barnsley L, Hall S, White M, Smidt N, et al. Non-steroidal anti-inflammatory drugs (NSAIDs) for treating lateral elbow pain in adults. Cochrane Database Syst Rev 2001;(4):CD003686
4) Smidt N, Assendelft WJ, van der Windt DA, Hay EM, Buchbinder R, Bouter LM. Corticosteroid injections for lateral epicondylitis: a systematic review. Pain 2002;96:23–40
5) Assendelft W, Green S, Buchbinder R, Struijs P, Smidt N. Tennis elbow. Clin Evid 2004;(11):1633–44
6) Paoloni JA, Appleyard RC, Nelson J, Murrell GA. Topical nitric oxide application in the treatment of chronic extensor tendinosis at the elbow: a randomized, double-blinded, placebo-controlled clinical trial. Am J Sports Med 2003;31:915–20













