Lumbar discography (discogram / diskogram) is a diagnostic procedure performed by fellowship-trained interventional pain physicians. It is usually ordered by spine surgeons in order to determine if a patient’s severe axial low back pain is caused by their lumbar disc disease (internal disc derangement) seen on MRI.
The suspected diseased and painful discs are tested with a single control level. The control disc is one that looks healthy on MRI and is not expected to be a pain generator for that patient.
If concordant pain is found in a particular disc, a spine surgeon will then perform a discectomy and fusion.
Indications
- Degeneration of Lumbar or Lumbosacral Intervertebral Disc (Lumbar Internal Disc Derangement)
- ICD-9 code: 722.52 “Lumbar/lumbosacral disc degeneration”
- ICD-10 code: M51.36 and M51.37 “Other intervertebral disc degeneration” (lumbar and lumbosacral, respectively)
CPT codes
- 62290 “Injection procedure for discography, EACH level; lumbar“
- 62291 “Injection procedure for discography, EACH level; cervical or thoracic“
- 72295 “Discography, lumbar, radiological supervision and interpretation” – EACH level
- 72285 “Discography, cervical or thoracic, radiological supervision and interpretation” – EACH level
- Note: Bill for EACH discogram level and EACH level of interpretation (don’t forget the -51 modifier).
- 99144 – moderate sedation (IV) – first 30 minutes (requires presence of another trained person to monitor the patient’s consciousness and vitals)
- 99145 – moderate sedation (IV) – each additional 15 minutes
- Fluoroscopic guidance is included in the above codes. Do NOT bill 77003 separately.
- Remember to bill for the J-codes for the radiopaque contrast as well.
Patient Position
- Prone
 Materials Needed
Materials Needed
- Gloves – sterile
- ChloraPrep (at least 10-ml)
- Band-aid – small, round
- Micro-bore plastic tubing (6-inch) – for injecting the lidocaine when the clearance between the needle hub and C-arm intensifier is too tight.
- Needles
- 27-gauge, 1.25″ – for skin numbing
- 25-gauge, 3.5″ – for numbing a tract down to the superior articular process (SAP)
- 22-gauge, 7″ – for entering the discs. One for each disc.
- Syringes
- (2) 10-ml plastic syringes (1% lidocaine)
- (1) 3-ml plastic syringe (bupivacaine 0.5%) – for injecting a small amount into each painful disc before removing the needles.
- Manometer: I have only used the Stryker manometer, which allows me to measure the volume injected and the digital display of intradiscal pressures.
- Injectables
- 1% lidocaine (20-ml)
- 0.5% bupivacaine (3-ml)
- Omnipaque 240 or 300: Put a maximum of 2-ml in each disc
- Prophylactic antibiotics
- The American Society of Regional Anesthesia (ASRA) recommended in 2006: pdf source link
- Cefazolin: 1-2 g IV 30 minutes before discogram, OR, 1-10 mg/ml with intradiscal contrast
- Clindamycin: 600-mg IV 30 minutes before discography, OR, 7.5 mg/ml with intradiscal contrast. For patients with cephalosporin allergies.
- Vancomycin: 1 g IV over 60 minutes before discogram. For patients who are MRSA carriers.
- Definitely no consensus on this topic, but below are examples of what some pain docs do.
- Example #1: IV before the procedure: 1-gram Ancef (cefazolin) IV before the procedure. Intradiscal: 3-ml clindamycin (450-mg) in 15-ml Omnipaque
- Example #2: Intradiscal only: 600-mg clindamycin (Cleocin) in 50-ml Omnipaque 300
- Example #3: Intradiscal only: 150-mg clindamycin (1-ml) with 9-ml Omnipaque
- Research Findings: “…IV or intradiscal antibiotics during discography have NOT been conclusively shown to decrease the rate of discitis over sterile technique alone.” (1)
- The American Society of Regional Anesthesia (ASRA) recommended in 2006: pdf source link
- Sedation medications
- Typically, 2-mg of Versed (midazolam) and sometimes 50-micrograms of fentanyl is needed. If in an ASC, might as well use some propofol too.
Technique, tips, and more
- Curve the needle tip slightly away from the opening of the needle. This has made the biggest difference for me in getting to center of the L5/S1 disc when you can’t oblique the C-arm enough because of the iliac crest getting in the way; really helps to curve medially once you pass the SAP.
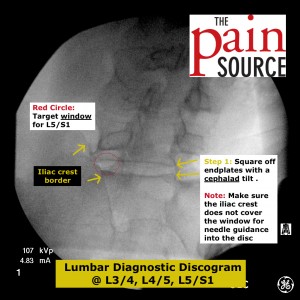
- Fluoroscopy tips:
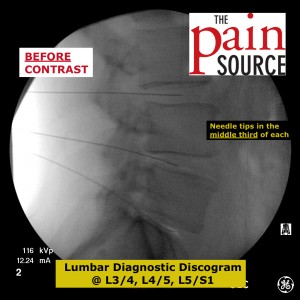
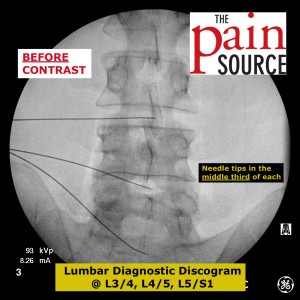
- First, square off the superior and inferior end-plates of each disc you target.
- Then, oblique toward the side you will enter (I go for the opposite of the patient’s most painful side).
- Ideal oblique angle: Get the SAP to the center of the disc. If you can get this, do not use much of a curve to the needle.
- Go slowly past the SAP so you can quickly pull back and adjust the needle if you tap the exiting nerve root.
- When you get to the disc, your tactile feedback will notice a distinct consistency change (“thick” resistance).
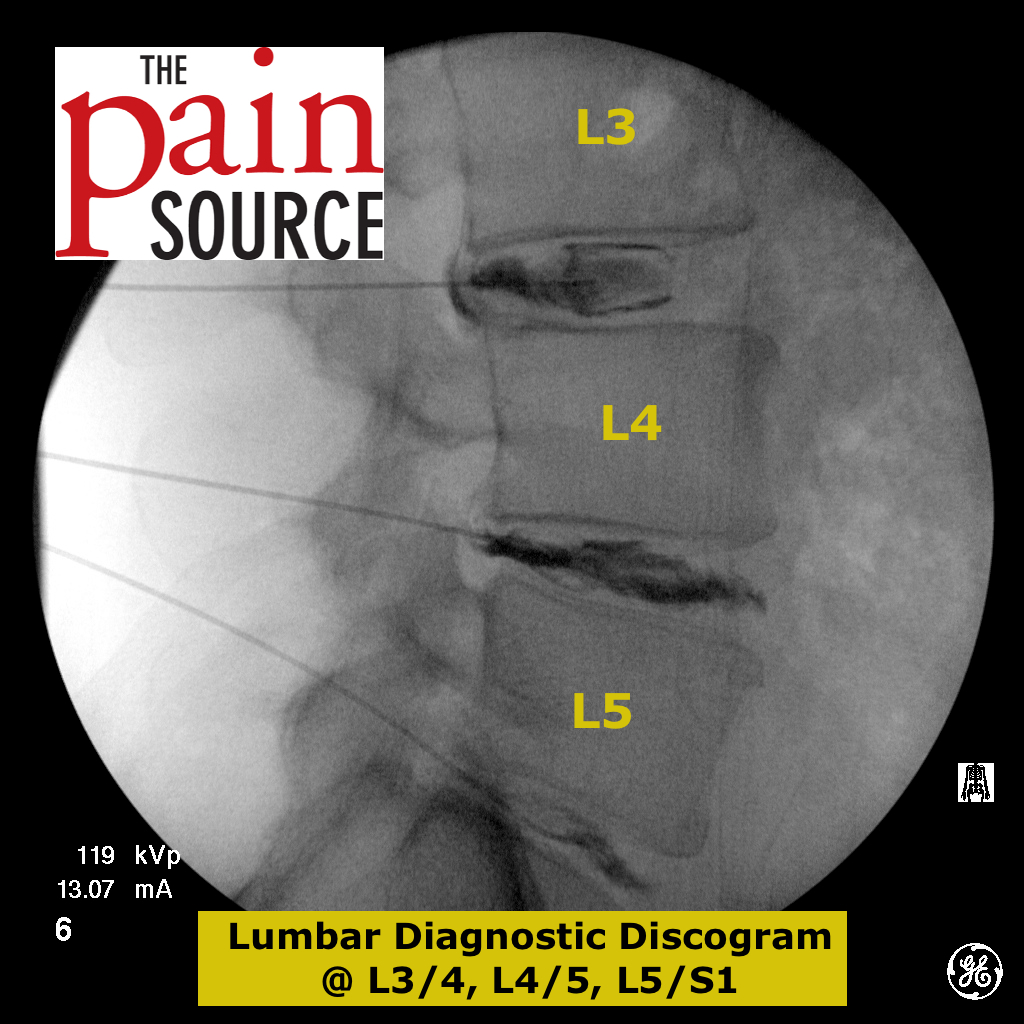
- Advance all needles through the discs with a lateral fluoroscopic view. Once the tip is in the middle third, check AP view to confirm it is in the middle third in that view too.
- Inject the contrast into the discs with the lateral view as well.
- Check the AP view at the end to see extravasation laterally too.
- Concordant pain
- It is NOT about pain during the procedure, it is all about CONCORDANT pain.
- The patient needs to clearly know that concordant pain is what you are looking for, not just vague “pressure pain”.
- The PAIN must be in the same location and be of the same quality.
- Tip: Limit the total contrast in each disc to 2-ml in order to limit the intradiscal pressures and false-positives in normal discs.
- Tip: Limit the intradiscal pressures to 100 mmHg in order to limit false-positives.
- Post-procedure CAT scan
- Some surgeons require a CT scan after the procedure in order to more clearly see the extent of extravasation of the contrast.
- I feel this is NOT needed, as the fluoroscopic images should be clear enough. An additional CT scan exposes the patient to more radiation, and also increases the total cost of each discogram.
- BUT, some surgeons want that extra detail from a CAT scan.
Four Conditions For A Positive Test – all must be met (opinion)
- Pain is concordant with the patient’s usual symptoms (same location and quality)
- Pain at low intradiscal pressures (less than 100 mmHg)
- Abnormal MRI findings and extravasation of contrast injected
- Control disc was not painful (when injected with up to 2-ml contrast and up to 100 mmHg)
Literature / Research
1) The prevention of discitis during discography. Spine J. 2009 Nov;9(11):936-43.