By Chris Faubel, MD —
PM&R. 2009 Aug;1(8):719-22.
The significance of multifidus atrophy after successful radiofrequency neurotomy for low back pain.
Dreyfuss P, Stout A, Aprill C, Pollei S, Johnson B, Bogduk N.
Department of Rehabilitation Medicine, University of Washington, 21108 NE 129th CT, Woodinville, WA 98077, USA. pauldreyfuss@gmail.com
http://www.ncbi.nlm.nih.gov/pubmed/19695523
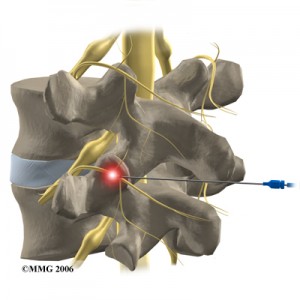
**picture to the right courtesy of eorthopod.com
ABSTRACT
OBJECTIVE: To determine the presence of lumbar multifidus atrophy and pain after successful lumbar medial branch radiofrequency neurotomy for zygapophysial joint mediated pain.
DESIGN: A prospective observational analysis of 5 patients who had undergone successful unilateral radiofrequency neurotomy (RFN) of the lumbar medial branch divisions of the lumbar dorsal rami. At 17 to 26 months after RFN, 3 blinded radiologists evaluated the relative composition and size of the multifidus muscle at different segmental levels on lumbar magnetic resonance imaging (MRI). They were asked to determine the lesioned levels by evidence of multifidus atrophy. The accuracy of predicting the correct side and level lesioned was evaluated.
SETTING: Private spine practice in Tyler, Texas.
PATIENTS: Five patients who had unilateral lumbar medial branch RFN for proven lumbar zygapophysial joint-mediated pain were selected.
INTERVENTIONS: MRI of the lumbar spine at a mean of 21 months (range, 17-26) after successful lumbar RFN.
OUTCOME MEASURES: Multifidus atrophy on a lumbar MRI, pain assessment and use of cointerventions.
RESULTS: Diffuse lumbar multifidus atrophy was detectable with MRI. However, radiologists could not reliably predict the side and segments lesioned. Despite denervation of the multifidus, at 12 months after RFN all subjects had ongoing pain relief and did not require or request additional treatment.
CONCLUSIONS: This preliminary study provides evidence that successful medial branch RFN for lumbar zygapophysial-mediated pain does cause initial denervation but no discernable segmental atrophy of the multifidus at long-term follow-up. Previous denervation and diffuse atrophy in these subjects was not associated with pain.
MY THOUGHTS
EDUCATIONAL POINTS:
- The multifidi (the deep back muscles) run from the mamillary process (MP) of one level, to the spinous process (MP) of a vertebrae 1-4 segments above (ex: L3-L5 to L2 SP)
- Thought to be innervated by the medial branch of the dorsal primary ramus of the level that attaches to the spinous process (L2 medial branch, in the example above)
- Though this has been challenged, “The lumbar multifidus muscle in polysegmentally innervated”: http://www.ncbi.nlm.nih.gov/pubmed/11155540
- But this is from a single case report
- Although, since the medial branch innervates the facet joint at it’s exiting level AND the one below, it stands to reason that that medial branch may also innervate two levels of multifidi
- Though this has been challenged, “The lumbar multifidus muscle in polysegmentally innervated”: http://www.ncbi.nlm.nih.gov/pubmed/11155540
- Multifidus atrophy has long been associated with low back pain [with the atrophy being thought of as the cause, and the pain seen as the effect] – this has NOT been proven
- It has therefore been thought by some that ablation of the medial branch would cause denervation of the multifidi, and therefore result in more low back pain
- Note: What they found in this study goes against that thinking
NEGATIVES:
- Small sample size
- No pre-RFN MRI – would be nice to see before and after images
- The MRI reading of atrophy was performed 17-26 months after the radiofrequency neurotomy – plenty of time for reinnervation of the multifidi, and therefore regrowth
- Only one RFN was performed in a two-year span. Would the atrophy had been more obvious with repeated RFN??
- No knowledge whether the patients went through physical therapy
BOTTOMLINE:
- These five patients underwent radiofrequency neurotomy, had evidence of multifidi denervation via EMG, then had atrophy at those levels no more than any other non-denervated level…and no increase in low back pain















Just a thought in glancing at the abstract – atrophy is found also in patients with LBP dennervation or not. I am not sure its possible to generate a cause effect relationship in this very complex issue.
The theory is also to RFA the sensory aspect with testing prior to RFA. The nerve is not completely destroyed, re; the motor aspect is in the DRG is theoretically not affected, while there may be atrophy to say if it was related to treatment you would need pre-procedure MRI. I am suprised they didn’t include them and as mentioned already– 5 patients?? Why could they have not included more, I am sure they were available.
With RFA, the sensory AND motor fibers in the medial branch of the dorsal primary ramus are destroyed. The sensory testing prior to ablation/neurotomy is to make sure the needle is near the medial branch. The motor testing is to make sure you’re nowhere near the ventral ramus going down the leg.
You’re correct, multifidus atrophy is found in chronic back pain suffers, but the argument against RFA has been that the interventional pain physicians are actually making the patient worse in the long run. This study showed that denervation that was present 6 wks after the neurotomy, was either not present or not discernably different that other levels that didn’t have RFA. You’re right though, pre-MRI imaging would have been great. And the small sample size was silly. But I still like the study in general. Great pilot study at least. Maybe someone can expand on it some day.
thanks for the reply
My initial comment was not clear- sorry about that. To clarify- Yes I agree both motor & sensory are affected as part of the RFA. But NOT motor from the ventral nerves. THe medial br. does supply the deep fascicles of the multifidus at that level of innervation. Bogduk’s dissection study also acclaims the multifidii are not multi-level innervated as what is commonly believed. The Medial branch of the dorsal primary ramus also innervates interspinalis and posterior spinal ligaments. By doing motor testing prior to RFA it is my impression you are trying to verify placement with stim of these medial branch innervated structures, multifidi contraction theoretically. Sensory stim is supposed to indicate coordinate pain as perceived by the patient. In addition I suppose you could say there is no stim of ventral roots but i don’t think that verifies placement parallel to the medial branch- only that you are NOT at the ventral roots. I am not a expert, but that’s my understanding of how its done. Sensory stim is probably more subjective measure, but an indication you are near the medial branch if you can’t see any contraction in the muscles at that level with motor stim. Not sure which is a better measure, probably both?
Regarding the study, could have been much better with the better design as mentioned. Their time probably could have been more effectively utilized and in the end producing a much better study with a better design. A case series (only 5 patients) is low on the scientific evidence scale. Nonetheless I suppose a good starting point as a pilot study. Ideally, a good study design produces good data and would be much better for discussion.
I just had RF on my facet joints today (L5-s1 to L3-L4). I am 34 prevous fitness nut, blah, blah, have had a Chronic low back pain for 7 years without any period free of pain.
Early on in my pain career Phyios told me my Multifidus is weak and tried to sell me on strengthening this muscle as a “cure” to my problem.
Are there other nerves that innervate the Multifidus and can strengthen of this muscle and other dorsal spinal muscles be acheived post RF.
Cheers.
Rob