By Chris Faubel, MD —
Understanding nerve injury classification is essential for prognostic value clinically.
Some basic anatomy, along with the two classification systems, and their corresponding EMG findings need to be learned and remembered.
Two classification systems exist (and are frequently tested in various exams):
- Seddon’s classification (neuropraxia, axonotmesis, neurotmesis)
- Sunderland’s classification (types 1-5)
To understand the systems, you must first review some basic nerve anatomy.
There are three connective tissue layers in the CNS and PNS.
- epineurium
- perineurium
- endoneurium
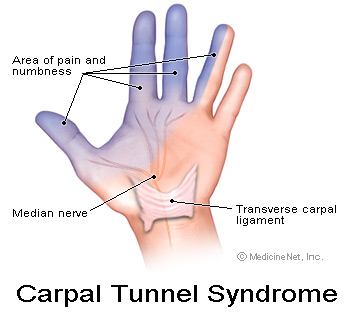
Individual nerve fibers (single axons) are covered with varying amounts of myelin and then covered by endoneurium. These individually wrapped nerve fibers are then grouped into bundles of fibers called fascicles, which are covered by perineurium. Finally, groups of fascicles are bundled together to form the peripheral nerve (such as the median nerve), which is covered by epineurium.
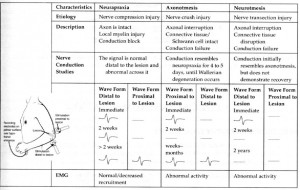
Seddon’s classification:
- Neuropraxia
- refers to local myelin injury with the axon still intact and functional
- motor > sensory fibers affected
- considered a temporary paralysis of the nerve fiber
- least severe injury
- usually from crush injury or ischemia
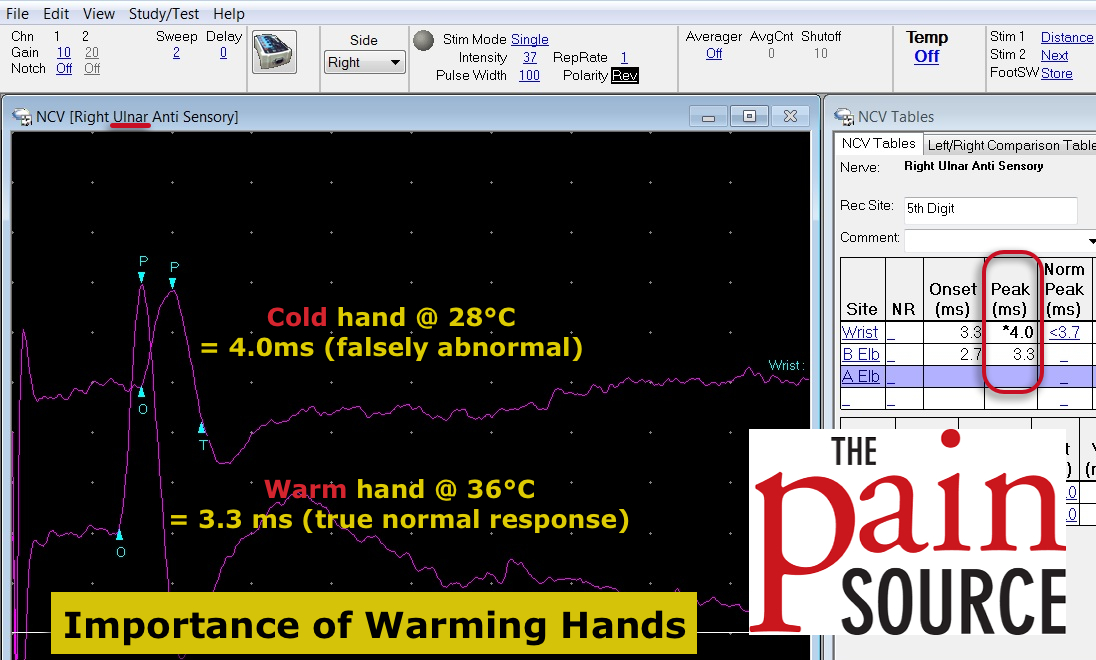
- Electrodiagnostic findings: (click the image to the right)
- note: normal CMAP amplitude distal to the lesion at day 10 is a “good” sign –> diagnosis of mild neuropraxia instead of axonotmesis or neurotmesis
- Recovery: hours to months (avg 6-8 weeks)
- refers to local myelin injury with the axon still intact and functional
- Axonotmesis
- the axon and myelin is disrupted here, but the neuronal connective tissue remains intact (endo-, peri-, epineurium)
- more severe crush injury than that which causes neuropraxia
- Wallerian degeneration occurs because of loss of axoplasmic flow
- Electrodiagnostic findings: (click the image to the right)
- absent nerve conduction distal to the lesion
- decreased amplitude and recruitment immediately
- spontaneous potentials (positive sharp waves & fibrillations) in 2-3 weeks
- Regeneration (if neuronal coverings are intact) occurs at about 1.5-3mm/day
- Recovery: weeks to months
- Neurotmesis
- most severe form
- not only the axon, but also injury to the myelin, endoneurium, perineurium, and in the most severe case, the epineurium
- Electrodiagnostic findings: (click the image to the right)
- same as with axonotmesis
- note: clinically, neurotmesis and axonotmesis present the same (motor, sensory, autonomic paralysis, and muscle atrophy)
- surgical repair is typically needed
- Recovery: incomplete; imperfect
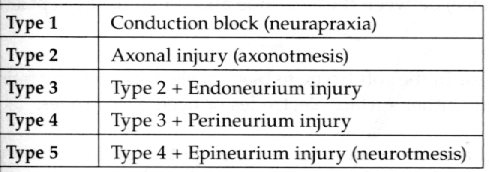
Sunderland’s classification:
- consists of 5 degrees of injury (further stratifying the extent of endo/peri/epineurium involvement)
- 1st degree
- essentially the same as neuropraxia
- 2nd degree
- same as axonotmesis
- 3rd degree
- axonotmesis, plus endoneurium disruptions
- 4th degree
- axonotmesis, plus endo- and perineurium disruptions
- 5th degree
- same as neurotmesis (complete transection)






[…] The Pain Source – Nerve Injury Classifications – Seddon’s and Sunderland’s – Your … […]
[…] Nerve injury – Google Blog Search by Ron Sombilon Gallery […]
[…] The Pain Source – Nerve Injury Classifications Seddon's and … […]