By Chris Faubel, MD —
Pes anserine bursitis is an inflammation of the pes anserinus bursa, leading to pain over the proximal anteromedial tibia.
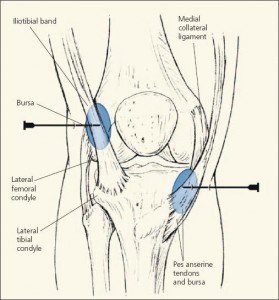
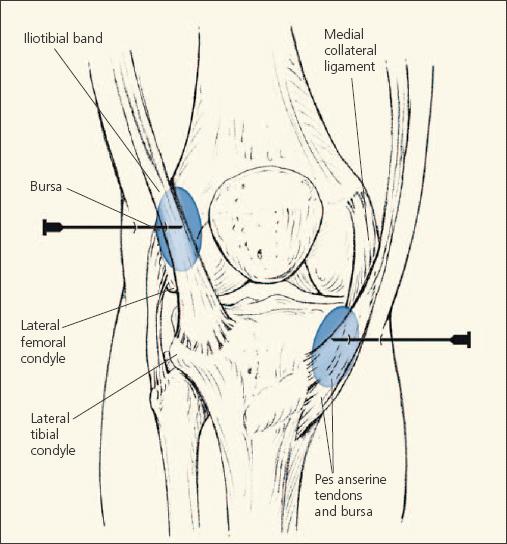
Pes anserinus bursa
- 4-5 cm distal to the anteromedial tibial joint line
- Lies just deep to the conjoint tendon formed by three (3) tendons
- Sartorius
- Gracilis
- Semitendinosus
- Insertion of the medial collateral ligament (MCL) and the medial tibia lies deep to the pes anserine bursa
Pes anserine bursa lies between the conjoint tendon of three muscles (superficially), and the medial collateral ligament and tibia (deep).
Presentation / Physical Exam Findings
- Pain at proximal anteromedial tibia 4-5 cm below the medial joint line
- Swelling (local) at that same location
- Patients frequently state they can’t sleep on their side without a pillow or other padding between their knees
Cause
- Repetitive friction over the bursa
- Valgus stress
- Sports activities with lots of pivot-shifts (soccer, football, tennis, etc)
- Valgus stress
- Direct trauma to the bursa
More common in:
- Females (larger Q-angle)
- Runners and other athletes with tight hamstrings
- Patients with
- Osteoarthritis, rheumatoid arthritis, diabetes mellitus, obesity
Diagnosis
- History and physical exam findings
- Computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound (US) are NOT usually helpful
- One case report has been found to show usefulness of musculoskeletal ultrasonography in the diagnosis of acute pes anserine bursitis [2]
- Usually, cases with large, swollen bursa seen on imaging, are clear cut and don’t require the need for expensive imaging technology
- ICD-9 code: 726.61 “pes anserinus tendinitis or bursitis”
- ICD-10 code: M70.5 “other bursitis of knee”
Treatment
- Ice or heat
- Stretching the thigh adductors and hamstrings
- Therapeutic ultrasound
- Interferential current (IFC)
- Iontophoresis and phonophoresis
- NSAIDs
- Corticosteroid injections
- Either performed blindly or via US-guidance
- Finnoff et al. [1] from the Mayo Clinic published at study which showed US-guided injections have a higher degree of accuracy (compared to “blinded” injections): 92% to 17% accuracy
- Either performed blindly or via US-guidance
Ultrasound-guided injections for the pes anserine bursa have a higher degree of accuracy than “blinded” injections.
Learn about the pes anserine steroid injection technique and tips HERE.
———————————————————–
REFERENCES:
1. Finnoff JT, Nutz D, Henning PT, Hollman JH, Smith J. Accuracy of Ultrasound-Guided versus Unguided Pes Anserinus Bursa Injections. PM&R 2010;2:732-739
2. Valley VT, Shermer CD. Use of musculoskeletal ultrasonography in the diagnosis of pes anserine tendinitis: A case report. The Journal of Emergency Medicine 2001:20;1:42-45














Why does us make such a difference?
I’ll post an article tomorrow that shows even after locating the middle of the bursa via ultrasound, the accuracy of performing the injection without US-guidance is only 50%, whereas it’s 100% with US.
You basically go straight down from point of maximal tenderness, hit bone (tibia), then back off a couple millimeters and inject. The problem is when you back off too much or not enough and the injectate doesn’t make it into the bursa.
I am surprised that US is not beneficial in diagnosis.
I re-edited the post and added a couple more remarks about imaging. CT, MRI, and diagnostic ultrasound can be helpful, but the cases are usually obvious enough to not need the expensive studies. MRI has been the imaging of choice though. A diagnostic trial of lidocaine injected into the bursa is quicker and less expensive. But of course with an acute valgus injury, with pain over the area of the pes anserine bursa, an MRI should be ordered to r/o other causes, like an MCL tear (and other terrible triad pathology common with that mechanism of injury).