
By Chris Faubel, M.D. –
Radiopaque contrast agents are used by pain physicians during fluoroscopically-guided injections and other pain procedures (kyphoplasty, discography). Their use is essential for confirming needle tip placement for eventual corticosteroid/local anesthetic administration, and to rule out inadvertent intravascular placement of the needle.
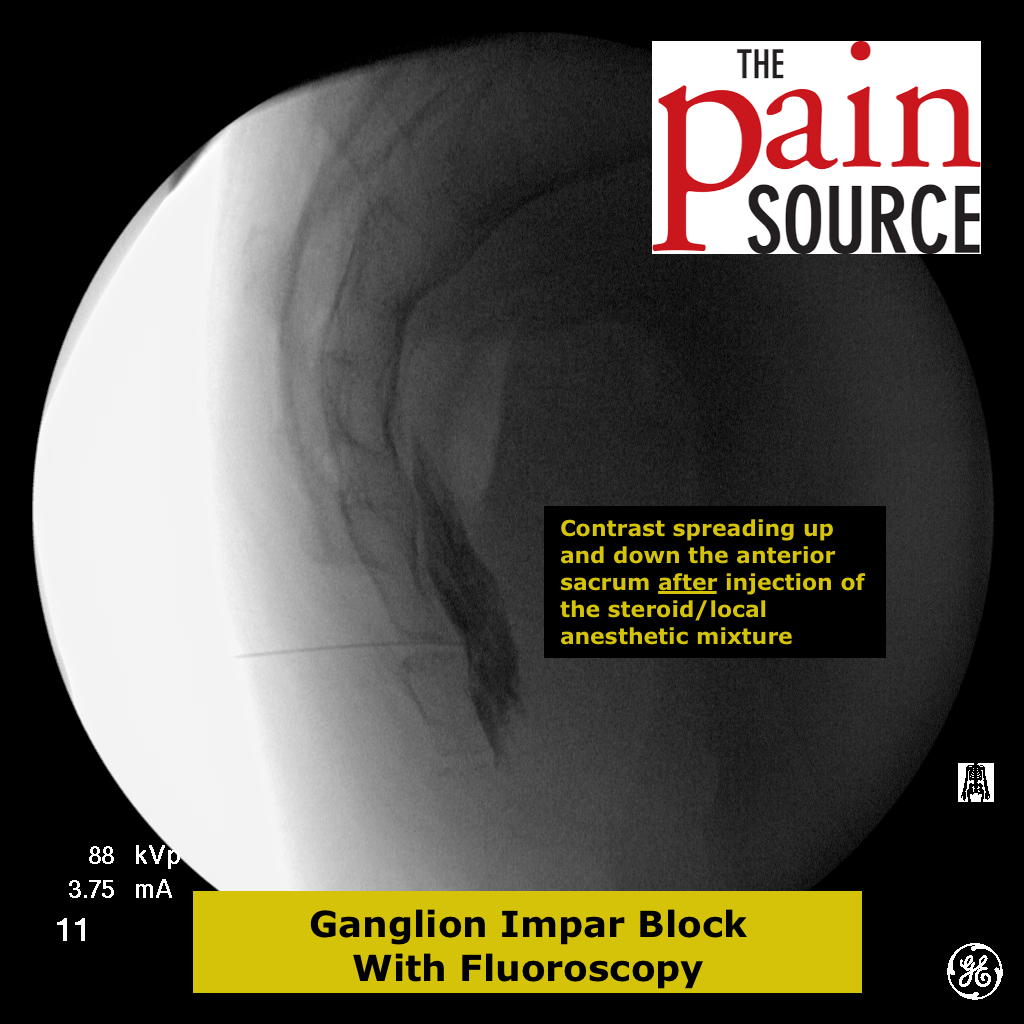
The contrast agents are radiopaque because of the iodine content in the solution. This iodine doesn’t allow penetration of x-rays, and therefore shows up as blackness (opaque) on the fluoroscopy monitor. Because it is more black than other structures being x-rayed, it is easy to visualize the spread of the contrast agent. This spread then allows the pain physician to know where the injectate (usually a corticosteroid and anesthetic) will also flow.
These radiocontrast agents can be divided into two categories: 1) Non-ionic. 2) Ionic
- The non-ionic agents are more hydrophilic, have a lower osmolality, and therefore produce fewer adverse effects (less risk of arachnoiditis or allergic response). Because of this, we only use non-ionic contrast agents.
The most commonly used contrast agents in pain medicine are iohexol (trade name = Omnipaque) and iopamidol (trade name = Isovue). These two solutions have a low concentration of iodine (200-300mg/ml), which makes them safe, yet still create good imaging contrast.
Clinical pearl: You can dilute the contrast agent with sterile, normal saline (by up to 25%) and still get sufficient darkening when injected.
Allergies to Shellfish (shrimp, crawfish, lobster, crabs)
- It has long been medical folklore that patients allergic to shellfish, would also be allergic to iodinated contrast agents because both contained iodine, and therefore there would be cross-reactivity.
- It has since been shown that the antigenic property of shellfish is actually a particular protein, not the iodine. [1]
- Injecting a small volume of non-ionic radiocontrast subcutaneously is NOT helpful in predicting whether that patient will have adverse reactions during a procedure.
- Mild reactions: urticaria (raised, itchy hives), pruritus; rhinorrhea; nausea, brief retching, and/or vomiting; diaphoresis; coughing; and dizziness.
- Moderate reactions: more vomiting, wider spread urticaria, mild bronchospasm, facial edema, hypotension
- Severe reactions: hypotension, severe bronchospasm, laryngeal edema, pulmonary edema, seizures, syncope, and death.
- All of the above are much more common with ionic contrast agents, not the nonionic agents we use in pain medicine.
- A very large case study in Japan in 1990 (337,647 cases), compared high-osmolar ionic contrasts to low-osmolar nonionic agents (like the Omnipaque and Isovue above). They found that severe adverse drug reactions to the contrast occurred in 0.22% of the ionic and only 0.04% of the nonionic contrast media. [2]
- In a large prospective study, the incidence of severe reactions was found to be 0%. [3]. However, in this same study, adverse effects of any severity was seen in 0.7% of patients.
- Patients with a seafood allergy have a slightly greater risk of having an adverse reaction (of any severity) to IV contrast. But it should be noted that this correlation was only shown with ionic contrast (which we don’t use), and that the increased risk is roughly the same as patients with allergies to eggs, milk, chocolate, strawberries, or those with asthma. Also, 85% of patients with a seafood allergy had no adverse reaction at all to the ionic IV contrast. [7]
- For patients with a true history of severe allergic reaction after a prior nonionic contrast administration, gadolinium contrast (usually used as MRI contrast) can be used safely and effectively [4].
- Some physicians recommend just pretreating patients that are high-risk for adverse reactions, or have had adverse reactions in the past.
- Three pretreatment regimen examples:
- Oral prednisone 20-50 mg, ranitidine (Zantac) 50 mg, and diphenhydramine 25-50 mg orally 12-24 hours prior to exposure by injection. An additional 25 mg of diphenhydramine can be given by IV immediately before contrast injection. [5]
- Methylprednisolone 32mg orally 12 hours and 2 hours before the injection. [6]
- Oral prednisone 50mg at 13, 7, and 1 hour before contrast injection, with Benadryl 50mg IV, IM, or PO, 1 hours before the contrast. [6]
- 12 hours before: oral prednisone 50mg; 2 hours before: oral prednisone 50mg and Benadryl 50mg [8]
References:
1) Andreas L. Lopata, and Samuel B. Lehrer. New Insights Into Seafood Allergy. Curr Opin Allergy Clin Immunol. 2009;9(3):270-277.
2) Katayama H, Yamaguchi K, Kozuka T, et al. Adverse reactions to ionic and nonionic contrast media. A report from the Japanese Committee on the Safety of Contrast Media. Radiology. Jun 1990;175(3):621-8.
3) Wolf GL, Arenson RL, Cross AP. A prospective trial of ionic vs nonionic contrast agents in routine clinical practice: comparison of adverse effects. AJR Am J Roentgenol. May 1989;152(5):939-44.
4) Safriel Y, Ali M, Hayt M, Ang R. Gadolinium use in spine procedures for patients with allergy to iodinated contrast–experience of 127 procedures. AJNR Am J Neuroradiol. 2006 Jun-Jul;27(6):1194-7.
5) Anthony H Wheeler. Therapeutic Injections for Pain Management. Medscape.com. Aug 3, 2011.
6) Pradeep Chopra and Howard Smith. Contrast Agents for the Interventional Pain Physician. Pain Physician. Vol. 7, No. 4, 2004
7) Beaty AD, Lieberman PL, Slavin RG. Seafood allergy and radiocontrast media: are physicians propagating a myth? Am J Med. 2008 Feb;121(2):158.e1-4.
8) http://www.radiology.ucsf.edu/patient-care/patient-safety/contrast/iodinated/premedication








Nice article. Succinct and informative!