By Chris Faubel, MD —
Does the chronic use of opiates/opioids/narcotics lead to testosterone deficiency?
- YES!! Testosterone deficiency has been observed in both males AND females taking pain-relieving narcotics for their chronic pain. [1,2]
How does this happen?
- First you must have a basic understanding of how testosterone is produced in the body.
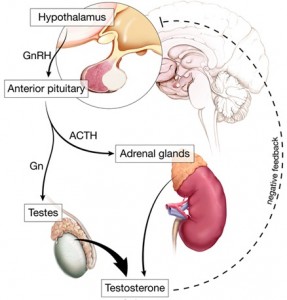
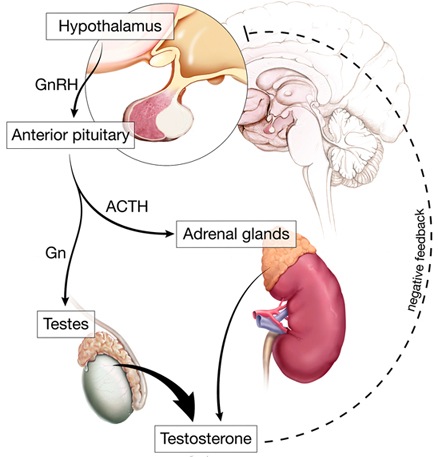
- By the testes (#1 way) – see the image to the right
- Testosterone is primarily made in the testicles by way of hormones from the hypothalamus and anterior pituitary
- Gonadotropin-releasing hormone (GnRH) is released by the hypothalamus, which then stimulates the anterior pituitary to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH). The FSH and LH then leads to testosterone production by the testes.
- By the adrenal glands
- GnRH also stimulates the pituitary to release (ACTH), which then tells the adrenals to make testosterone.
- By the testes (#1 way) – see the image to the right
- Theories of how chronic pain and chronic opioid use causes testosterone deficiency
- Opioid suppression of GnRH
- Most common cause
- Suppression of GnRH and LH/FSH due to the stress of severe, uncontrolled pain over time
- Opioid suppression of GnRH
What are the signs and symptoms of testosterone deficiency in patients?
- Poor pain control
- Low libido
- Erectile dysfunction (Impotence)
- Depression
- Lack of energy
- Poor sleep
- Compression fractures
Is testosterone related to pain perception?
- Yes…at least in rats.
- Forman et al. found that castrated rats responded to painful stimuli quicker, and that treatment with testosterone propionate caused a normalization of the response. [3]
- What about in humans?
- Boston University is currently recruiting participants to see if testosterone administered to men with opioid-inducted hypogonadism leads to a change in their pain perception, pain sensitivity in response to noxious stimuli, and changes in the requirement of opioids.
How is this testosterone deficiency tested?
- Morning (8am – 11am) serum TOTAL testosterone level
- Serum levels of testosterone peak in the morning .
- Some consider free testosterone to be a better judgment of testosterone level, because it is the unbound, bioavailable portion (most involved with libido and erectile dysfunction). But others feel the protein portion is more critical for pain management purposes.
- Other tests to consider
- LH level to determine if the low testosterone is primary (low testosterone; high LH) or secondary (low testosterone; low LH)
- Prolactin level
- Bone densitometry – to check if osteoporotic
How is opioid-induced androgen deficiency treated?
- This may be determined by which version the insurance company pays for.
- Cheapest
- Injectable testosterone is the cheapest
- Compounding pharmacies may make topical creams and gels for a similar price
- Table of commercially available preparations
- A trial can be given with 200-mg (1-ml) of injectable testosterone (or one-week supply of commercial testosterone) to see if symptoms improve within one week
- Side effects of testosterone replacement
- The severe, highly-publicized effects of anabolic steroids in athletes is from use of extremely high doses
- Link to table with list of potential effects
- For the most part, acne (males) and beard growth (females) is the tip off that too much testosterone is being administered, and a reduction is needed.
—————————————————–
REFERENCES:
- Katz N, Mazer NA. The impact of opioids on the endocrine system. Clin J Pain. 2009 Feb;25(2):170-5
- Daniell, H.W. Opioid-induced androgen deficiency. Current Opinion in Endocrinology & Diabetes. 2006 June;13(3):262-266
- Forman et al. The response to analgesia testing is affected by gonadal steroids in the rat. Life Sci. 1989;45(5):447-54
- Tennant F, Lichota L. Testosterone Replacement In Chronic Pain Patients. Practical Pain Management. July/August 2010. Vol 10, Issue 6, Pages 12-15






What is the normal range of total testosterone in the body?
The normal ranges of testosterone vary throughout life, between genders, and between different laboratories.
Opioid suppression of GnRH
Stress/uncontrolled pain-suppression of GnRH and LH/FSH
Also decreased level of activity due to pain…
What happens if you wean off the chonic opioids and how long does it take for the neuroendocrine system to reach homestasis before you re-tst the patient?